Framing Cancer Survivors’ Access to and Use and Disposal of Prescribed Opioids Within the Opioid Epidemic
Purpose: To explore cancer survivors’ access to and use and disposal of opioids in the context of the opioid epidemic.
Participants & Setting: Community-based recruitment strategies were employed for individuals aged 18 years or older who were previously diagnosed with cancer, completed cancer treatment within the past five years, or were cancer free, and who were prescribed opioids for cancer-related pain.
Methodologic Approach: This qualitative study used semistructured interviews. Data were analyzed using applied thematic analysis techniques.
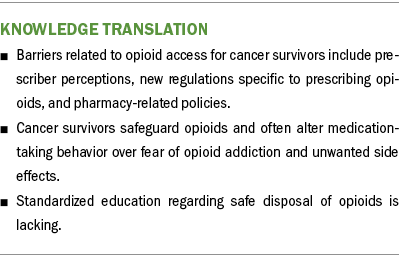
Findings: Themes included the following: (a) restrictive policies affecting opioid access and supply, (b) decreased opioid use because of concerns of addiction and other opioid-related side effects, and (c) lack of clarity on safeguarding and disposal of opioids.
Implications for Nursing: Cancer survivors may encounter barriers to opioid access, alter medication-taking behavior over fear of addiction and side effects, and face inadequate education regarding proper disposal of opioids. Nurses can advocate for appropriate access to prescribed opioids, assess opioid-taking behavior, provide education regarding storage and disposal, and implement educational interventions accordingly.
Jump to a section
About 18.2 million cancer survivors are living in the United States, and that number is expected to steadily increase to more than 22.5 million in the next decade (National Cancer Institute, 2022). The increase in the number of survivors is largely influenced by earlier cancer detection and advancements in cancer treatments (American Cancer Society, 2016, 2019). Regardless of their cancer type or treatment trajectory, cancer survivors can experience several long-term effects of the disease or treatment, including pain (Glare et al., 2014; Sanford et al., 2019). “Cancer survivor” can be defined in many ways. For the purpose of this article, a cancer survivor is defined as an individual who has completed curative treatment or who has transitioned to maintenance or prophylactic treatment.
Pain is a common symptom experienced by cancer survivors (Glare et al., 2014). It is estimated that 40%–50% of survivors experience chronic pain despite the completion of curative cancer treatment (Kurtin & Fuoto, 2019; Sanford et al., 2019; van den Beuken-van Everdingen et al., 2007). Pain, which can be related to the cancer itself or cancer treatment, can present as somatic, visceral, and/or neuropathic (Glare et al., 2014; Levy et al., 2008). For example, widespread tumor progression can compress the surrounding structures, organs, tissues, or nerves, causing pain. Pain can also result from tissue damage from surgery, radiation therapy, chemotherapy, and various procedural tests (Glare et al., 2014; Levy et al., 2008). Pain syndromes, such as phantom breast pain or pain related to breast reconstruction after mastectomy, can be chronic (Levy et al., 2008; Lovelace et al., 2019). Individuals completing radiation therapy may experience conditions, such as brachial plexopathy, which can present as neuropathic pain or paresthesia lasting long after treatment (Levy et al., 2008). Chemotherapy can damage the nerves in the extremities and lead to peripheral neuropathy (Colvin, 2019; Glare et al., 2014). Some chemotherapies and hormone therapies can cause arthralgia and myalgia (Glare et al., 2014; Seguin et al., 2017). Chemotherapy- or radiation therapy–induced mucositis and infections may also cause pain that affects nutrition (Elad & Yarom, 2019). Pain from mucositis can persist after the condition is healed and treatment has ended (National Cancer Institute, 2019). Regardless of the cause, unrelieved pain can cause disturbance of sleep patterns, poor appetite leading to nutritional deficits, declined functioning, and decreased quality of life (Brown et al., 2014; Elad & Yarom, 2019; Glare et al., 2014; Paice & Ferrell, 2011; Sanford et al., 2019).
Opioids are often prescribed as an initial treatment modality for pain among cancer survivors (Glare et al., 2014). Although nonopioid alternatives, such as exercise, acupuncture, and psychosocial interventions, are recommended because of issues with long-term opioid use (Glare et al., 2014), survivors have noted that these methods are not always covered by health insurance plans (Marshall et al., 2022). The current opioid epidemic has led several federal agencies and professional organizations, including the Centers for Disease Control and Prevention (Dowell et al., 2016) and the American Society of Clinical Oncology (Paice et al., 2016), to recognize and respond to safe opioid prescribing practices. Safe opioid storage and disposal have also been noted as a concern. McCauley et al. (2013) reported that more than half of study participants were uninformed about proper storage and disposal of unused prescription opioids. This lack of knowledge often led to misuse of opioids, such as using for purposes not prescribed or sharing medication. Similar findings of a lack of education on safe opioid storage and disposal related to unintended misuse have been reported (Lewis et al., 2014; Lipari & Hughes, 2017; Reddy & de la Cruz, 2019). In addition, the opioid epidemic has changed the way prescription opioids are perceived by the community, including patients with a history of cancer who experience chronic pain (Tyson, Chavez, Lake, et al., 2021; Tyson, Chavez, Lubrano, et al., 2021).
As cancer survivors transition from active cancer treatment to survivorship care, chronic pain management can be overlooked, and pain needs may not be met (Chao et al., 2020), particularly within the context of the opioid epidemic. Suboptimal pain management has been reported among cancer survivors, which can negatively affect quality of life (Hamood et al., 2018; Janah et al., 2020). Many factors can contribute to inadequate pain control, including healthcare provider training and pain assessment skills, provider beliefs and biases toward pain and prescription pain medication, and hesitancy to prescribe opioids because of stricter laws and regulations (Kurtin & Fuoto, 2019; Kwon, 2014; Paice & Ferrell, 2011). Healthcare system–related issues that can negatively affect pain management among cancer survivors include inconsistencies in opioid prescribing practices among clinicians, insurance barriers (e.g., noncoverage of alternative pain treatments), and regulatory restrictions placed on opioid prescriptions (Kwon, 2014; Scarborough & Smith, 2018). In addition, racial, ethnic, and socioeconomic disparities specific to the access, assessment, evaluation, and treatment of pain have been described, which result in undermanaged and unresolved pain (Becker et al., 2011; Dovidio & Fiske, 2012; Maly & Vallerand, 2018; Scarborough & Smith, 2018; Tait & Chibnall, 2014).
Purpose
This study aimed to explore the access to and use and disposal of opioids among cancer survivors prescribed these medications for pain in the context of the opioid epidemic. This research was developed after consulting with community partners who had direct relationships with cancer survivors who were prescribed opioids.
Methodologic Approach
Design, Participants, and Setting
This exploratory pilot study used individual in-depth qualitative interviews with survivors prescribed opioids for cancer-related pain. Community-based recruitment strategies were employed using purposive sampling. Participants were eligible if they met the following inclusion criteria: (a) diagnosed with cancer, (b) completed cancer treatment in the past five years, (c) currently considered cancer free, (d) prescribed an opioid for pain related to cancer or its treatment, and (e) aged 18 years or older. Participants were given a $30 gift card to compensate for their time in this study.
Flyers about the study that were approved by the University of South Florida Institutional Review Board and the H. Lee Moffitt Cancer Center Scientific Review Committee were distributed throughout community-based oncology centers and support groups in the Tampa Bay area and via social media. Interested participants were instructed to contact the principal investigator via email or telephone, who then screened interested participants for eligibility and obtained informed consent.
Procedures
Participants were called and interviewed by master’s-prepared graduate research assistants, who were trained on the study’s protocol by the principal investigator. Interviews lasted about 30–45 minutes and followed a semistructured format. Participant demographic and self-reported cancer and cancer treatment characteristics were collected.
The interview guide was developed with input from the study’s community advisory board, which consisted of experts in health disparities, cancer survivorship, nursing, public health, internal medicine, psychiatry, palliative care, and substance misuse. Having clinical expertise from fields such as nursing, medicine, and mental health was imperative to address the challenges surrounding cancer survivors’ access to and use and disposal of opioids prescribed for pain in the context of the opioid epidemic. The interview guide was initially pilot tested with one participant and then reviewed by members of the community advisory board to ensure appropriate flow and clarity of the questions. The following five domains were included in the interview guide:
- General health information (e.g., “How would you describe your general health status prior to being diagnosed with cancer and your general health status now?”)
- Cancer diagnosis and pain (e.g., “What do you do to alleviate pain? Who prescribes your pain medications?”)
- Perceptions of opioids (e.g., “What comes to mind when you hear the term ‘opioid’?”)
- Prescription opioids (e.g., “What type of opioid were you prescribed? Where do people typically store medications at home?”)
- Opioid adherence and monitoring (e.g., “Did you take the medication as prescribed by your doctor?”)
To confirm credibility, study participants were asked to clarify their responses if they were unclear to the interviewer. Interviews were performed until data saturation was met (Guest et al., 2006).
Data Analysis
All interviews were audio recorded and transcribed verbatim. Data were analyzed using applied thematic analysis techniques (Guest et al., 2011). Atlas.ti, version 8.0, was used to code data. Inter-rater reliability was set at a threshold of 0.8. In addition, a PhD-prepared researcher skilled in qualitative analyses completed an independent thematic analysis, and results were compared to increase the confirmability and reliability of findings. Descriptive statistics were used to analyze participant demographic and cancer-related characteristics.
Findings
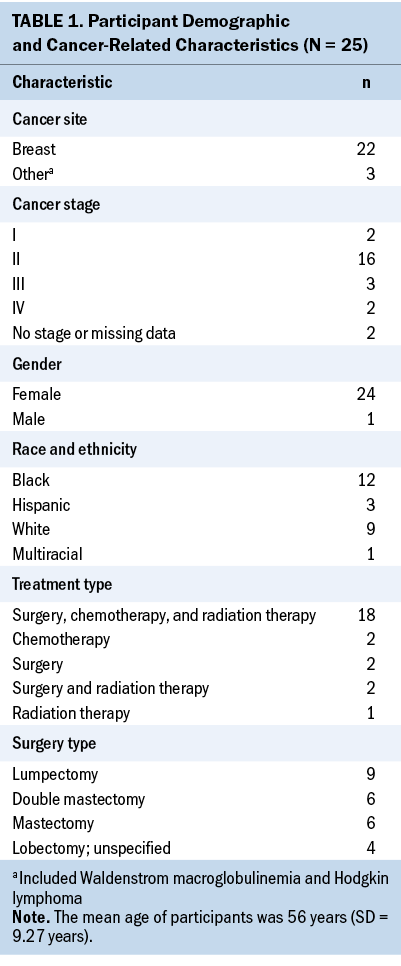
Twenty-five cancer survivors were interviewed (see Table 1). The sample consisted mostly of women (n = 24) with breast cancer (n = 22) and a stage II cancer diagnosis (n = 16). The mean age of participants was 56 years. Participants identified as Black (n = 12), White (n = 9), Hispanic (n = 3), or multiracial (n = 1). Study themes included the following: (a) restrictive policies affecting opioid access and supply, (b) decreased opioid use because of concerns of addiction and other opioid-related side effects, and (c) lack of clarity on safeguarding and disposal of opioids. The following sections present the study themes and participant quotes.
Theme 1: Restrictive Policies Affecting Opioid Access and Supply
Participants noted difficulty with obtaining opioids. Participants’ perceptions were that providers, such as oncologists, primary care physicians, and pain management physicians, were hesitant to write narcotic prescriptions for pain because of strict guidelines, despite the participants’ cancer diagnoses and treatment. According to participants, these restrictive policies were often associated with the opioid epidemic. For example, participant 19 (diagnosed in 2013) noted,
Pain medication is very hard to get. You have to really go to a doctor, and they really have to believe that you need it. She said that they have to put something that it’s acute or something on there for us to get the prescription filled now. She said that it was getting harder to get them filled than before because of all of the people abusing the system, taking it and not needing it.
Providers were unwilling to prescribe long-term prescriptions for patients and were conservative with prescribing opioids. Participant 13 (diagnosed in 2016) explained,
They did make a big point of “This is not a permanent thing. This is just to get you through.” The only thing they give you is your pills for your surgery or after surgery. The doctors really don’t prescribe you a lot. I think it was a 21-day prescription. They don’t give you enough where you’re really going to be selling them, and you’re not going to get another prescription.
Participant 18 (diagnosed in 2011) also recounted that their provider was “very conservative when he writes scripts, doesn’t put renewals.”
Several participants reported that when prescribed opioids for pain, they still faced difficulty in filling them and finding pharmacies that could supply the medication. Others had difficulty obtaining the medication because of stricter opioid-specific regulations and safety precautions. Some noted that physicians verbalized new licensing restrictions, which limited their ability to prescribe opioids. In addition, participants reported that new restrictions and securities at the pharmacies made it challenging to pick up their medication. Some pharmacies required the patients prescribed the medication to pick up the drug themselves, which was burdensome because they were in too much pain to drive or were too ill. As participant 2 (diagnosed in 2014) described,
They [the pharmacy] were really strict on who would be allowed. I was the only one allowed to fill it. You know what I mean? I specifically had to go pick it up, which is hard when you’re feeling like garbage.
Participant 1 (diagnosed in 2015) reported issues with accessing opioids and not being able to call ahead of time to ensure the pharmacy had the medication because of safety precautions, which was difficult when the patient was in pain and had to travel to different pharmacies looking for one that could fill the prescription:
The problem that I had was where to get them refilled. I wasn’t in a position just to get in a car and ride around. We actually called one pharmacy—the hospital didn’t have it, so we had to call a pharmacy to try to see if they actually have the drug. I didn’t want to just drive to—I just happen to call a pharmacy and ask about getting a prescription. What they told me is that the pharmacies will not tell you if they have the drug or not because of it being a controlled substance. They run into situations where they have that particular drug that they’ve had robberies or what have you. I was informed that it’s going to be tough for me to try to find the pharmacy that have it just by calling. I actually have to literally go to the pharmacy.
Despite having a prescription, new opioid regulations made it challenging to access opioids. Opioid prescriptions required different diagnosis codes, which sometimes delayed and inconvenienced participants. Participant 19 (diagnosed in 2013) illustrated,
The other week when I went to get my last prescription, the lady said to me at the pharmacy, “Oh, we can’t fill this. We have to call the doctor first.” I said to her, “Why do you have to call the doctor? I get this pill all the time here.” She said, “Oh, there was a new law since July 1.”
Theme 2: Decreased Opioid Use Because of Concerns of Addiction and Other Opioid-Related Side Effects
Participants verbalized being comforted in knowing that they had prescription opioids for pain control; however, they were cautious about the addictive nature of opioids and took their medication only as necessary. Participants reported using alternatives to opioids, such as oral and topical nonsteroidal anti-inflammatories, herbal and vitamin therapies, exercise, and meditation, as needed to supplement pain control. Participant 3 (diagnosed in 2016) shared,
Honestly, at that moment, I was quite happy with it because I was in such a severe pain, but I was also very cognizant of the fact that they can be addictive, so I was personally very, very careful with that. In fact, I still have about 60 or 55 of those pills left, and, for all this time, I only take it if I absolutely have to.
Participant 11 (diagnosed in 2016) added, “I did not want anything stronger than what I can buy over the counter. Because you see in the news about this whole opioid addiction, and I did not want to be dependent upon any type of drug.” Participant 1 (diagnosed in 2015) discontinued opioids because she feared she would become dependent on them: “That’s something I just didn’t want to have any addictions to or anything, so I came off of the hydromorphone.”
A majority of participants managed their opioid use depending on their experiences with side effects of the medication, often taking less medication than prescribed or discontinuing medication independently. For example, participant 8 (diagnosed in 2018) described stopping opioids because of side effects, “He did prescribe me some [oxycodone] as well, and I think I took those probably like two or three days, and then I told him that I discontinued taking it myself [because of nausea].” Participant 2 (diagnosed in 2014) added regarding decreasing her prescribed dose because of side effects of the medication, “I would take half because if I took a whole one, I was like a zombie for almost the entire day.” Participant 15 (diagnosed in 2013) noted that the side effects were almost as challenging as the pain itself: “I don’t like them because I know how I react, and the headaches that I get in between dosages [are] almost as worse than the pain that I’m trying to manage.”
Theme 3: Lack of Clarity on Safeguarding and Disposal of Opioids
Participants reported that they safeguarded opioids in locations other than medicine cabinets, including placing them in locked boxes or keeping them out of sight in closets or nightstands. Participants with children or grandchildren were particularly vocal about keeping opioids stored out of reach and noted that they worried about teenagers trying opioids because of media coverage of the opioid epidemic. Participant 25 (diagnosed in 2017) shared the following:
I keep mine up away from my children, and I keep mine off, away from people in general because I don’t really trust about my medications because you don’t really know a lot at times that a person is on the drug. Who knows? It’s a popular drug, and I believe that people that take it do get high. I keep my medications up. None but two people who know where my medicine is. They’re my granddaughter who takes care of me and myself.
Participant 26 (diagnosed in 2010) said, “Since my grandson was with me, it would always be out of sight, and, for the most part, it would be hidden in a box or something in my bedroom.” Participant 2 (diagnosed in 2014) shared,
I did not put them in my medicine cabinet, and I kind of hid them at the top of the closet behind some stuff so that if somebody came into my house, they wouldn’t know where they were. I hid them because I worry about my kids bringing a friend in the house.
Some participants reported a lack of trust in others and were careful not to share that they were prescribed an opioid, for fear that others would try to steal their medication. Participant 19 (diagnosed in 2013) said,
I don’t let people know that I take the drug first of all. I don’t. Because I don’t trust people. People can steal them from you just to be getting high and stuff like that, so I keep that kind of stuff locked up, and I don’t advertise that I take it.
Participants were uneducated regarding the safe disposal of opioids. This caused them to keep opioids in their homes or dispose of the medications incorrectly. Participants had been given a wide range of instructions that were neither consistent nor standardized. Participant 8 (diagnosed in 2018) shared, “I read somewhere saying, I think, you can flush down the commode.” Participant 22 (diagnosed in 1992) said, “You just drop them in the sink. What I do, if something doesn’t work, and I go back and I tell the doctor, ‘Listen, I put ammonia in mine and put the cap back on, so I’m fine.’”
Discussion
This study explored access to and the use and disposal of opioids among cancer survivors prescribed medications for pain in the context of the opioid epidemic. Opioid misuse was not reported among study participants. Participants noted that they self-adjusted their medications in reaction to perceptions of opioids and the opioid crisis. They also expressed concerns related to drug addiction, fear of death or dying, and undesirable side effects related to opioids. Many stated that they learned of the opioid crisis through the news or other media outlets, which heightened their fears and led to a reluctance to continue taking opioids for cancer pain. This left them at risk for ongoing and uncontrolled pain.
Participants reported difficulty obtaining access to opioids, which posed a barrier to proper pain management. However, despite the highly diverse sample, access did not differ among races or ethnicities, which contrasts with findings from other studies. For example, in a study exploring the ability of Black patients with cancer to access pain medications at their local pharmacy, about 51% reported problems getting their opioids filled. Of these patients, 28% had to wait days, and 24% had to return to the pharmacy multiple times (Jefferson et al., 2019).
State and federal regulations to combat the opioid epidemic have unintentionally contributed to pharmacies being more reluctant to store and fill opioid prescriptions, resulting in access barriers, which was a concern reported by participants in this study. Some pharmacies have limited the number of opioids they stock and have been reluctant to disclose to patients over the telephone whether they have the medication available. Some of the most reported barriers from pharmacies are concerns about diversion (82%), illicit use (90%), and shortage of opioids (67%) (Lal et al., 2019). Filling prescriptions at a hospital-based pharmacy may be more accessible, if feasible.
Cancer survivors who are prescribed opioids for pain need to understand that if they take their medication as prescribed and do not have risk factors, such as a history of substance misuse, the risk for addiction is low. Opioids can promote healing and restore physical function. Education regarding the safety and proper disposal of prescribed opioids was lacking among participants in this study. Participants seemed to be aware of the importance of safeguarding medication from others, including children and those who could potentially steal or misuse the medication. However, they did not always store their medication in a locked cabinet or container as recommended (Robeznieks, 2018); therefore, the opioids could have been accessible to others in the home. Such safeguarding of opioids could be affected by the opioid epidemic and fear instilled into cancer survivors by the news or other media outlets (National Cancer Institute, 2018). Many participants discussed the opioid epidemic during their interviews and described how this influenced their willingness to take their opioids as prescribed for fear of addiction.
Education is key to ensuring the safe handling, storage, and disposal of prescribed opioids. There is a lack of consistency and knowledge of safe storage and disposal of opioids not only among cancer survivors, but also among healthcare professionals (Odom-Forren et al., 2019; Reddy et al., 2014). In the current study, survivors received their opioid prescriptions from a variety of different sources, including oncologists, primary care physicians, and pain management physicians, which may have added to the lack of consistent knowledge regarding safe storage, handling, and disposal. Addressing opioid use, storage, and disposal at routine oncology visits can ensure education is received. In a previous study that implemented an educational program specific to the safe storage, use, and disposal of opioids in a comprehensive care center, those who received education were more aware of proper opioid disposal, less likely to share the prescription opioid with others, more aware of the danger of sharing opioids with others, more likely to use opioids as prescribed, less likely to store unused medication in the home, and more likely to keep opioids in a safe place that was either hidden or locked (de la Cruz et al., 2017). Another intervention to improve the safe disposal of opioids included designated disposal bags containing activated charcoal, which increased the safe disposal of unused opioids (Lawrence et al., 2019). Such interventions are feasible for nurses to implement in the oncology setting.
Several federal agencies provide recommendations for safe storage and disposal of opioids; however, nursing guidelines are lacking (Odom-Forren et al., 2019). In addition, guidelines from cancer-specific agencies note the need for safe storage and disposal, but there is no position statement describing what constitutes safe storage or disposal (National Comprehensive Cancer Network [NCCN], 2022; Paice et al., 2016). The U.S. Food and Drug Administration (FDA, 2021) recommends dropping off expired or unused opioids at a designated drug takeback facility as the first choice for disposal. National Drug Take Back Day occurs twice per year, in April and October, where temporary drug collection sites are set up in communities nationwide to assist with the safe disposal of prescription drugs. These sites are often held in local law enforcement agencies and may also be advertised by local waste management authorities. Permanent takeback collections are also housed in retail pharmacy chains, local pharmacies, and supermarkets. Locations can be searched on the Drug Enforcement Administration website or by calling the Registration Call Center.
If a drug takeback program is not available in a patient’s area, the FDA (2021) recommends methods to dispose at home. Because of the potential danger of some controlled substances, the FDA (2020) developed a flush list to identify which medications should be flushed down the toilet. For medications not on the flush list, it is recommended that patients throw them away in the household trash, following the directions at www.fda.gov/drugdisposal (FDA, 2020). The U.S. Department of Justice and Drug Enforcement Administration (2014) notes a broader range of acceptable disposal techniques, such as drug takeback events, mail-back programs, drug collection receptacles, and drop-offs at local law enforcement agencies. Other options include at-home drug disposal programs, which promote the proper deactivation of unused opioids (Deterra Drug Deactivation System, n.d.). These programs dispense organic and environmentally friendly pouches and containers that use activated carbon to deactivate the medications (Deterra Drug Deactivation System, n.d.). However, this method requires community distribution efforts and proper funding.
Limitations
Although this study had a diverse sample for qualitative analyses, there were some limitations. The qualitative nature of this study is not generalizable to larger populations. The sample was largely women with early-stage breast cancer, whose cancer treatment trajectory may differ from that of men with cancer, those with more advanced stages of cancer, or those with various cancer types. The sample was also not limited by cancer stage. Interviews with additional men and survivors with various cancers may lend more widespread perspectives. To the authors’ knowledge, the sample did not consist of individuals with a history of addictive behaviors, which could affect usage, storage, and disposal practices. In addition, the participants’ specific pain issues and use of opioids were not quantified. Time since cancer treatment was collected but not assessed.
Implications for Nursing
Nurses are at the forefront of pain and opioid use assessments. According to national guidelines, pain should be assessed at every visit (NCCN, 2022; Paice et al., 2016). Opioid use and effectiveness, as well as alternative pain treatments, should be evaluated (NCCN, 2022; Paice et al., 2016). Screening for potential opioid misuse and risk of misuse should be an active part of the nursing assessment (Teulings & Broglio, 2020). Nurses should also assess any adverse effects of opioid treatment that could alter medication-taking behavior or prompt a change in the treatment of pain. Patient satisfaction with pain control should be evaluated (NCCN, 2022). Nurses can address any fears of opioids and eradicate myths about opioid safety among cancer survivors (Battista et al., n.d.). In addition, any barriers to adequate pain control should be addressed and may require collaboration with interprofessional teams of oncologists, nurses, pharmacists, social workers, pain management physicians, psychologists, and addictive specialists (NCCN, 2022; Paice et al., 2016). These barriers include patients’ experiences when accessing legitimate prescriptions from their pharmacy. Nurses can educate pharmacists on patients’ experiences with and potential distress when filling legitimate opioid prescriptions, along with opportunities to provide patients with education regarding safe use of opioids and their rights when filling prescriptions (Brown et al., 2020).
Within this context, it is important for nurses to evaluate their own personal biases related to pain and pain management as these could negatively affect the implementation of nursing interventions. Patient and caregiver education is essential for safe handling, storage, and disposal of opioids. Prior to prescribing an opioid, assessment of past substance misuse or other addictive behaviors is recommended and should be ongoing. Education pertaining to the patients’ and caregivers’ identified needs should be accessible (NCCN, 2022; Paice et al., 2016). First, opioids should be stored in a secure location. Access to opioids can be a danger to others living in the home or visitors, with a risk for misuse or accidental overdose (de la Cruz et al., 2017). If patients are no longer using opioids for pain management, the unused opioids should be properly discarded, and a written list of locations for safe disposal should be provided to patients to ensure consistency with information. This information may vary from facility to facility based on site-specific policies and procedures. Nurses can assess pain and opioid use, storage, and disposal, and implement educational interventions as needed.
Conclusion
Chronic cancer pain management within the context of the opioid epidemic requires thorough assessment of patient knowledge, past experiences, and potential barriers. Cancer survivors may alter their medication-taking behavior by taking less medication than prescribed for fear of addiction to opioids, safeguard their opioid medication, or lack standardized education regarding proper disposal of opioids. Standardized education is needed to ensure proper opioid use, storage, and disposal of prescribed opioids.
About the Authors
Victoria K. Marshall, PhD, RN, is an assistant professor in the College of Nursing, Melody N. Chavez, MPH, is a doctoral candidate in the College of Public Health, and Khary K. Rigg, PhD, is an associate professor in the College of Behavioral and Community Sciences in the Department of Mental Health Law and Policy, all at the University of South Florida; Barbara Lubrano di Ciccone, MD, is an associate member of psychiatry and supportive care medicine at the H. Lee Moffitt Cancer Center; and Sahana Rajasekhara, MD, FAAHPM, is an associate professor in the College of Medicine in the Department of Oncologic Sciences, Andrea Efre, DNP, APRN, ANP, FNP-C, is an assistant professor in the College of Nursing, and Dina Martinez Tyson, PhD, MA, MPH, is an associate professor in the College of Public Health, all at the University of South Florida, all in Tampa. This research was supported, in part, by the Geographical Management of Cancer Health Disparities Program at the H. Lee Moffitt Cancer Center through funding from the National Cancer Institute Center to Reduce Cancer Health Disparities. Chavez, Rigg, and Martinez Tyson contributed to the conceptualization and design. Chavez and Rajasekhara completed the data collection. Chavez provided statistical support. Marshall, Chavez, and Martinez Tyson provided the analysis. All authors contributed to the manuscript preparation. Marshall can be reached at vkmarshall@usf.edu, with copy to ONFEditor@ons.org. (Submitted February 2022. Accepted June 18, 2022.)
References
American Cancer Society. (2016). Cancer treatment and survivorship facts and figures, 2016–2017. https://bit.ly/2HJtjnp
American Cancer Society. (2019). Cancer treatment and survivorship facts and figures, 2019–2021. https://bit.ly/3iQXImH
Battista, V., Haskamp, A., & Schreiner, E. (n.d.). Opioid pain management in serious illness [Webinar]. https://www.ons.org/webinars/opioid-pain-management-serious-illness-web…
Becker, W.C., Starrels, J.L., Heo, M., Li, X., Weiner, M.G., & Turner, B.J. (2011). Racial differences in primary care opioid risk reduction strategies. Annals of Family Medicine, 9(3), 219–225. https://doi.org/10.1370/afm.1242
Brown, J.H., Torres, H.P., Maddi, R.D., Williams, J.L., Dibaj, S.S., Liu, D., & Bruera, E. (2020). Cancer patients’ perceived difficulties filling opioid prescriptions after receiving outpatient supportive care. Journal of Pain and Symptom Management, 60(5), 915–922. https://doi.org/10.1016/j.jpainsymman.2020.06.015
Brown, M.R., Ramirez, J.D., & Farquhar-Smith, P. (2014). Pain in cancer survivors. British Journal of Pain, 8(4), 139–153. https://doi.org/10.1177/2049463714542605
Chao, Y.-H., Wang, S.-Y., & Sheu, S.-J. (2020). Integrative review of breast cancer survivors’ transition experience and transitional care: Dialog with transition theory perspectives. Breast Cancer, 27(5), 810–818. https://doi.org/10.1007/s12282-020-01097-w
Colvin, L.A. (2019). Chemotherapy-induced peripheral neuropathy: Where are we now? Pain, 160(Suppl. 1), S1–S10. https://doi.org/10.1097/j.pain.0000000000001540
de la Cruz, M., Reddy, A., Balankari, V., Epner, M., Frisbee-Hume, S., Wu, J., . . . Bruera, E. (2017). The impact of an educational program on patient practices for safe use, storage, and disposal of opioids at a comprehensive cancer center. Oncologist, 22(1), 115–121. https://doi.org/10.1634/theoncologist.2016-0266
Deterra Drug Deactivation System. (n.d.). Personal use: Destroying unused medications at home is easy with Deterra. https://deterrasystem.com/personal-use
Dovidio, J.F., & Fiske, S.T. (2012). Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102(5), 945–952. https://doi.org/10.2105/ajph.2011.300601
Dowell, D., Haegerich, T.M., & Chou, R. (2016). CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA, 315(15), 1624–1645. https://doi.org/10.1001/jama.2016.1464
Elad, S., & Yarom, N. (2019). The search for an effective therapy and pain relief for oral mucositis. JAMA, 321(15), 1459–1461. https://doi.org/10.1001/jama.2019.3269
Glare, P.A., Davies, P.S., Finlay, E., Gulati, A., Lemanne, D., Moryl, N., . . . Syrjala, K.L. (2014). Pain in cancer survivors. Journal of Clinical Oncology, 32(16), 1739–1747. https://doi.org/10.1200/jco.2013.52.4629
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
Guest, G., MacQueen, K.M., & Namey, E.E. (2011). Applied thematic analysis. Sage.
Hamood, R., Hamood, H., Merhasin, I., & Keinan-Boker, L. (2018). Chronic pain and other symptoms among breast cancer survivors: Prevalence, predictors, and effects on quality of life. Breast Cancer Research and Treatment, 167(1), 157–169. https://doi.org/10.1007/s10549-017-4485-0
Janah, A., Bouhnik, A.D., Touzani, R., Bendiane, M.-K., & Peretti-Watel, P. (2020). Underprescription of step III opioids in French cancer survivors with chronic pain: A call for integrated early palliative care in oncology. Journal of Pain and Symptom Management, 59(4), 836–847. https://doi.org/10.1016/j.jpainsymman.2019.10.027
Jefferson, K., Quest, T., & Yeager, K.A. (2019). Factors associated with black cancer patients’ ability to obtain their opioid prescriptions at the pharmacy. Journal of Palliative Medicine, 22(9), 1143–1148. doi.org/10.1089/jpm.2018.0536
Kurtin, S., & Fuoto, A. (2019). Pain management in the cancer survivor. Seminars in Oncology Nursing, 35(3), 284–290. https://doi.org/10.1016/j.soncn.2019.04.010
Kwon, J.H. (2014). Overcoming barriers in cancer pain management. Journal of Clinical Oncology, 32(16), 1727–1733. https://doi.org/10.1200/jco.2013.52.4827
Lal, A., Bai, J., Basri, D., & Yeager, K.A. (2019). Pharmacists’ perspectives on practice, availability, and barriers related to opioids in Georgia. American Journal of Hospice and Palliative Medicine, 36(6), 472–477. https://doi.org/10.1177/1049909118815440
Lawrence, A.E., Carsel, A.J., Leonhart, K.L., Richards, H.W., Harbaugh, C.M., Waljee, J.F., . . . Cooper, J.N. (2019). Effect of drug disposal bag provision on proper disposal of unused opioids by families of pediatric surgical patients: A randomized clinical trial. JAMA Pediatrics, 173(8), e191695. https://doi.org/10.1001/jamapediatrics.2019.1695
Levy, M.H., Chwistek, M., & Mehta, R.S. (2008). Management of chronic pain in cancer survivors. Cancer Journal, 14(6), 401–409. https://doi.org/10.1097/PPO.0b013e31818f5aa7
Lewis, E.T., Cucciare, M.A., & Trafton, J.A. (2014). What do patients do with unused opioid medications? Clinical Journal of Pain, 30(8), 654–662. https://doi.org/10.1097/01.ajp.0000435447.96642.f4
Lipari, R.N., & Hughes, A. (2017). How people obtain the prescription pain relievers they misuse. Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services. https://www.samhsa.gov/data/sites/default/files/report_2686/ShortReport…
Lovelace, D.L., McDaniel, L.R., & Golden, D. (2019). Long-term effects of breast cancer surgery, treatment, and survivor care. Journal of Midwifery and Women’s Health, 64(6), 713–724. https://doi.org/10.1111/jmwh.13012
Maly, A., & Vallerand, A.H. (2018). Neighborhood, socioeconomic, and racial influence on chronic pain. Pain Management Nursing, 19(1), 14–22. https://doi.org/10.1016/j.pmn.2017.11.004
Marshall, V.K, Chavez, M., Efre, A., Lake, P.W., Rigg K.K., Lubrano, B., . . . Tyson, D.M. (2022). Barriers to adequate pain control and opioid use among cancer survivors: Implications for nursing practice. Cancer Nursing. Advance online publication. https://doi.org/10.1097/NCC.0000000000001126
McCauley, J.L., Back, S.E., & Brady, K.T. (2013). Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addictive Behaviors, 38(6), 2230–2235. https://doi.org/10.1016/j.addbeh.2013.01.019
National Cancer Institute. (2018). The opioid epidemic and cancer pain management: A conversation with Dr. Judith Paice. https://www.cancer.gov/news-events/cancer-currents-blog/2018/opioid-cri…
National Cancer Institute. (2019). Oral complications of chemotherapy and head/neck radiation (PDQ®)—Patient version. https://www.cancer.gov/about-cancer/treatment/side-effects/mouth-throat…
National Cancer Institute. (2022). Statistics and graphs. Office of Cancer Survivorship. https://cancercontrol.cancer.gov/ocs/statistics
National Comprehensive Cancer Network. (2022). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Adult cancer pain [v.2.2022]. https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf
Odom-Forren, J., Brady, J., Rayens, M.K., & Sloan, P. (2019). Perianesthesia nurses’ knowledge and promotion of safe use, storage, and disposal of opioids. Journal of Perianesthesia Nursing, 34(6), 1156–1168. https://doi.org/10.1016/j.jopan.2019.04.005
Paice, J.A., & Ferrell, B. (2011). The management of cancer pain. CA: A Cancer Journal for Clinicians, 61(3), 157–182. https://doi.org/10.3322/caac.20112
Paice, J.A., Portenoy, R., Lacchetti, C., Campbell, T., Cheville, A., Citron, M., . . . Bruera, E. (2016). Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 34(27), 3325–3345. https://doi.org/10.1200/JCO.2016.68.5206
Reddy, A., & de la Cruz, M. (2019). Safe opioid use, storage, and disposal strategies in cancer pain management. Oncologist, 24(11), 1410–1415. https://doi.org/10.1634/theoncologist.2019-0242
Reddy, A., de la Cruz, M., Rodriguez, E.M., Thames, J., Wu, J., Chisholm, G., . . . Bruera, E. (2014). Patterns of storage, use, and disposal of opioids among cancer outpatients. Oncologist, 19(7), 780–785. https://doi.org/10.1634/theoncologist.2014-0071
Robeznieks, A. (2018, September 6). 5 tips for safely storing opioids at home. American Medical Association. https://www.ama-assn.org/delivering-care/opioids/5-tips-safely-storing-…
Sanford, N.N., Sher, D.J., Butler, S.S., Xu, X., Ahn, C., Aizer, A.A., & Mahal, B.A. (2019). Prevalence of chronic pain among cancer survivors in the United States, 2010–2017. Cancer, 25(23), 4310–4318. https://doi.org/10.1002/cncr.32450
Scarborough, B.M., & Smith, C.B. (2018). Optimal pain management for patients with cancer in the modern era. CA: A Cancer Journal for Clinicians, 68(3), 182–196. https://doi.org/10.3322/caac.21453
Seguin, C., Kovacevich, N., & Voutsadakis, I.A. (2017). Docetaxel-associated myalgia–arthralgia syndrome in patients with breast cancer. Breast Cancer, 9, 39–44. https://doi.org/10.2147/bctt.s124646
Tait, R.C., & Chibnall, J.T. (2014). Racial/ethnic disparities in the assessment and treatment of pain: Psychosocial perspectives. American Psychologist, 69(2), 131–141. https://doi.org/10.1037/a0035204
Teulings, L., & Broglio, K. (2020). Opioid misuse risk: Implementing screening protocols in an ambulatory oncology clinic. Clinical Journal of Oncology Nursing, 24(1), 11–14. https://doi.org/10.1188/20.CJON.11-14
Tyson, D.M., Chavez, M.N., Lake, P., Gutierrez, A., Sherry, P., Rigg, K.K., . . . Pabbathi, S. (2021). Perceptions of prescription opioid medication within the context of cancer survivorship and the opioid epidemic. Journal of Cancer Survivorship, 15(4), 585–596. https://doi.org/10.1007/s11764-020-00952-1
Tyson, D.M., Chavez, M.N., Lubrano, B., Lake, P., Gutierrez, A., Marshall, V.K., . . . Rajasekhara, S. (2021). Understanding cancer survivors’ educational needs about prescription opioid medications: Implications for cancer education and health literacy. Journal of Cancer Education, 36(2), 215–224. https://doi.org/10.1007/s13187-021-01957-9
U.S. Department of Justice and Drug Enforcement Administration. (2014). Title 21—Code of federal regulations: Disposal. https://www.govinfo.gov/content/pkg/USCODE-2014-title21/html/USCODE-201…
U.S. Food and Drug Administration. (2020). Drug disposal: FDA’s flush list of certain medicines. https://www.fda.gov/drugs/disposal-unused-medicines-what-you-should-kno…
U.S. Food and Drug Administration. (2021). Safe opioid disposal—Remove the Risk outreach toolkit. https://www.fda.gov/drugs/safe-disposal-medicines/safe-opioid-disposal-…
van den Beuken-van Everdingen, M.H.J., de Rijke, J.M., Kessels, A.G., Schouten, H.C., van Kleef, M., & Patijn, J. (2007). Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Annals of Oncology, 18(9), 1437–1449. https://doi.org/10.1093/annonc/mdm056


