Correlates of Physical Health Comorbidities Among Adult Female Cancer Survivors in South Korea
Objectives: To determine correlates of comorbidities in adult female Korean cancer survivors.
Sample & Setting: This cross‐sectional study used data from the 2017–2019 Korea National Health and Nutrition Examination Survey. The study sample consisted of adult female Korean cancer survivors (N = 609) aged 19 years or older.
Methods & Variables: Comorbidities were assessed using an adapted Charlson Comorbidity Index (CCI). Bivariate and multivariate linear regression analyses were conducted to identify correlates of comorbidities. Data were collected on sociodemographic characteristics, cancer-related characteristics, and comorbidities.
Results: The mean adapted CCI score was 2.4. Type of cancer and years since diagnosis were significant correlates of comorbidity. Other significant correlates included high body mass index, physical inactivity, low income, having less than a college education, being a former or current smoker, and having never smoked.
Implications for Nursing: Many correlates of comorbidities in adult female Korean cancer survivors are consistent with those reported in other countries, including in the United States. Nurses can assess and educate cancer survivors on modifiable risk factors to prevent health comorbidities in cancer survivorship care.
Jump to a section
Cancer incidence has been increasing in recent years in South Korea (subsequently referred to as “Korea”) (Jung et al., 2019). Because of improved cancer screening and treatment, there has also been an increase in the number of cancer survivors, defined as those who have ever received a cancer diagnosis (Jung et al., 2019). However, general medical care and support for Korean cancer survivors are less than optimal (Shin et al., 2013). For instance, although the United States has specific health behavior recommendations for cancer survivors (Rock et al., 2020), Korea does not have any established guidelines (Shin et al., 2013). Because of environmental, cultural, and behavioral differences, guidelines in the United States cannot be automatically applied to Korea without further evidence of their potential value to the Korean population (Shin et al., 2013). In addition, Korea does not have laws similar to the Comprehensive Cancer Care Improvement Act in the United States, nor does the country have a reimbursement system or community-level care delivery system similar to that in place in the United States for cancer survivors (Shin et al., 2013).
Medical practitioners and patients with cancer in Korea report deficits in cancer survivorship care. Patients report insufficient consultation time with their oncologists (Shin, Park, et al., 2012). In addition, patient surveys indicate that Korean cancer survivors are less likely than those without cancer to receive adequate diabetes management and less likely to adhere to antihypertensive medication, possibly because of a lack of systematic care and guidelines (Shin et al., 2014; Shin, Park, et al., 2010).
Korean oncology practitioners report a lack of resources and evidence-based survivorship care guidelines, and Korean healthcare providers in various disciplines identify the lack of an interprofessional shared care system, limited community resources, and poorly tailored long-term survivorship cancer care to be issues that currently undermine survivorship care in Korea (Chan et al., 2017; Lim et al., 2018). Korean physiatrists also report that cancer survivors are not receiving sufficient rehabilitation care, likely because of a limited understanding of cancer rehabilitation and an inadequate cooperative referral system (Yang et al., 2015). As a result of this insufficient care, many Korean cancer survivors suffer from physical comorbidities, defined as physical diseases that coexist with their cancer history, and nearly a quarter of adult Korean five-year cancer survivors die of noncancer causes (Hwangbo et al., 2018; Oh et al., 2020; Park, Han, et al., 2021; Porta, 2014; Shin, Ahn, et al., 2010).
Researchers have emphasized a need to understand differences among cancer survivors from various racial and ethnic groups (Wen et al., 2014). Korean cancer survivors tend to experience significantly more susceptibility to physical fatigue than their U.S. counterparts (Jang et al., 2020). Although aerobic physical activity and strength exercise have been associated with lower risk of comorbidities in Korean cancer survivors (Kang et al., 2018), the authors’ search of the literature did not identify any factors related to risk of physical comorbidities in these survivors. To inform a comprehensive care system and guidelines for cancer survivors in Korea, it is critical to understand the current level of the most common long-term physical health comorbidities that cancer survivors experience and patient characteristics related to those comorbidities.
The authors’ previous study identified sociodemographic characteristics, modifiable risk factors, and cancer-related variables correlated with physical comorbidities in adult U.S. cancer survivors (Park & Strauss, 2019). Deimling et al. (2005) found that adult female cancer survivors have a greater number of comorbidities and worse health and functioning than adult male cancer survivors. Because of this finding, the authors’ previous U.S. study examined correlates of physical comorbidities in adult female cancer survivors separately (Park & Strauss, 2019). Adult female Korean cancer survivors are more likely to perceive that they received uncoordinated cancer care than adult male Korean cancer survivors (Shin et al., 2020). Individuals receiving such uncoordinated care have an increased risk of new comorbidities, so correlates of physical comorbidities among adult female Korean cancer survivors also merit separate attention (Shin et al., 2020). The purpose of this study is to examine characteristics associated with comorbidities in adult female Korean cancer survivors based on those previously identified in adult U.S. cancer survivors.
Methods
The Korea National Health and Nutrition Examination Survey
Data from the 2017–2019 Korea National Health and Nutrition Examination Survey (KNHANES), collected by the Korea Disease Control and Prevention Agency, were used for this cross-sectional study. Every year, KNHANES collects nationwide data from noninstitutionalized civilians in Korea. Data are collected through health interviews, health examinations, and a nutrition survey. Deidentified public data are available through the KNHANES website (Korea Disease Control and Prevention Agency, n.d.). Kweon et al. (2014) provide additional details about KNHANES. The current study’s analyses used data on body mass index (BMI), sociodemographic characteristics, medical conditions, and physical activity from health examinations and questionnaires.
Sample Selection and Quality Control
KNHANES uses a complex three-stage probability sample design. First, primary sample units are selected from a sampling frame of all census blocks or resident registration addresses. Then, targeted households are sampled from each primary sample unit. Finally, individuals in the household are asked to participate in the survey. IBM SPSS Complex Samples, version 26.0, is used to calculate statistics and minimize bias when extrapolating findings to the noninstitutionalized Korean civilian population. Potential bias is also limited by using various approaches to reduce measurement errors. Among these approaches are periodic staff training, the use of a standardized environment, and regular calibration of equipment (Kim, 2014). This study used the following criteria for inclusion: (a) being female, (b) being an adult aged 19 years or older, and (c) having been diagnosed with one or more cancers.
Amended Charlson Comorbidity Index
An amended version of the Charlson Comorbidity Index (CCI) was used in this study. The CCI was originally developed to identify significant comorbid health conditions and to predict one-year mortality risk in patients with these conditions (Charlson et al., 1987). Quan et al. (2011) updated the CCI with new weighted scores to better represent improved treatment in chronic disorders. Versions of the CCI have been widely used in research in diverse populations, including among cancer survivors in Korea (Woo et al., 2010). Among adult Korean cancer survivors who underwent surgery for gastric cancer, versions of the CCI demonstrated good test–retest reliability using Spearman rho coefficients (Hwang et al., 2009). Good predictive validity was also demonstrated in association with noncancer mortality in adult Korean men aged younger than 65 years who had prostate cancer and underwent radical prostatectomy (Lee et al., 2014). In the current study, the CCI was used to identify comorbidities that may significantly affect health outcomes in cancer survivors.
Quan et al.’s (2011) updated CCI was adapted for the current study (subsequently termed the “adapted CCI”) for relevance to adult cancer survivors. This adaptation enabled the use of data collected in the 2017–2019 KNHANES. Because some comorbid conditions have a weighted score of 0 (e.g., myocardial infarction, peripheral vascular disease, cerebrovascular disease, peptic ulcer disease, diabetes without chronic complications), they were not included in the score for the adapted CCI. The current study was performed in cancer survivors, so malignancy and metastatic solid tumors were excluded from the adapted CCI. In addition, KNHANES does not collect data on some components of the updated CCI (e.g, congestive heart failure, dementia, diabetes with chronic complications, hemiplegia or paraplegia, liver disease, AIDS/HIV). Consistent with the work of others, these components were not included in the adapted CCI (Noh et al., 2019). Age was incorporated into the adapted CCI as it is an important factor in comorbid health conditions (Sarfati et al., 2011). Thus, the adapted CCI included the following comorbidities: chronic pulmonary disease (asthma); rheumatologic disease (rheumatoid arthritis); and renal disease (renal disease), each scoring 1 point; and mild liver disease (hepatitis B, hepatitis C, cirrhosis), scoring 2 points. Age was divided into five categories, each assigned the following point values: aged 40 years or younger, 0 points; aged 41–50 years, 1 point; aged 51–60 years, 2 points; aged 61–70 years, 3 points; and aged 71 years or older, 4 points. Points for comorbid conditions and age categories were added together to calculate the total adapted CCI score. The possible range for total adapted CCI scores was 0 to 9, with higher scores indicating more comorbidity.
Potential Predictors of Adapted CCI Scores
Potential predictors identified in the U.S. research literature were used for the current study. Sociodemographic characteristics included education (college and above versus less than college) and household income. In KNHANES, data on household income are collected on a four-point Likert-type scale ranging from low income to high income. For the current study, these data were coded as low income or non–low income. Race and ethnicity were excluded because the study population was comprised entirely of ethnic Korean individuals.
Modifiable characteristics included BMI, physical activity, and cigarette smoking. Because Asian racial and ethnic groups tend to have differences in body composition from other racial and ethnic groups, the World Health Organization (WHO) suggests different BMI categories for assessing BMI in the Asian population (WHO Expert Consultation, 2004). Consistent with the WHO recommendations, a BMI of 23 or greater was considered overweight or obese in this study. In the current study, BMI was coded as normal weight versus overweight or obese.
Consistent with previous research among Korean cancer survivors, physical activity was examined according to guidelines established by the American Cancer Society (ACS) (Koh et al., 2019; Park, Lee, et al., 2021). The ACS recommends at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous-intensity activity per week, or a prorated combination of the two (Rock et al., 2020). KNHANES collects information on weekly physical activity related to work or leisure according to intensity (moderate or vigorous), frequency (number of days per week), and duration (number of hours and minutes). Participants were classified as either meeting or not meeting the ACS guidelines.
In the current study, cigarette smoking was coded as former or current smoker versus never smoker. When asked if they had “ever smoked in their lifetime,” participants who answered “never smoked” were classified as never smokers. When asked about their current smoking status, participants who indicated that they “smoke every day” or “smoke sometimes” were classified as current smokers, and those who “smoked in the past but do not smoke currently” were classified as former smokers.
Cancer-related variables were also analyzed as potential predictors of comorbidity. These variables were type of cancer (stomach, colon, breast, cervical, thyroid, or other), diagnosis with two or more of these cancer types, and years since initial cancer diagnosis.
Statistical Methods
Adult female cancer survivors who had complete data on all variables were included in the study (N = 609). The KNHANES sampling plan uses stratification, clustering, and unequal selection probabilities, so correct analysis of the data requires the use of statistical software able to compute the sample weights and design variables that the KNHANES data provide. IBM SPSS Complex Samples, version 26.0, was used to obtain valid point estimates, standard errors, and confidence intervals in the current study’s analyses, which were performed according to the KNHANES data analysis guidelines (Korea Disease Control and Prevention Agency, 2019; West et al., 2018). Using IBM SPSS Complex Samples, version 26.0, it was possible to extrapolate findings to produce unbiased cross-sectional estimates for the adult female Korean population with a previous cancer diagnosis.
Descriptive statistics (means, standard errors, and proportions) were used to describe potential predictors. Bivariate linear regression analyses were used to examine the independent relationships of each of the potential predictors with the adapted CCI score. To determine whether there would be multicollinearity in the subsequent multivariate logistic regression analysis to predict the adapted CCI score, the authors examined bivariate correlations between potential predictors. If there were no large correlations between potential predictors, a purposeful selection process could be used to choose variables for inclusion in the multivariate regression analysis. If there were large correlations, adjustments would need to be made to the predictors so that they would be independent. To not exclude any important variables in the multivariate model, variables that were found to have a p value of less than 0.2 in the bivariate analyses were selected to be entered into the multivariate linear regression analysis (Mickey & Greenland, 1989). Backward elimination was then used to retain the statistically significant predictors (p < 0.05) in the final multivariate regression model for the adapted CCI score.
Human Participants Consideration
Informed consent was obtained from all individual participants at the time of their enrollment in KNHANES. This study received an exemption from the institutional review board of Hunter College, the City University of New York.
Results
Sample Description
The study sample was comprised of 609 adult female Korean respondents, aged 19 years or older, who were previously diagnosed with cancer. The study sample of 609 individuals was more than adequate for the proposed regression analyses. Design effects were all less than 1.1 for each of the potential predictors of the adapted CCI score. Thus, on average, no more than 1.1 times as many sample cases are needed than if a simple random sample were used in the analysis (Shackman, 2001). For example, using NCSS Power Analysis and Sample Size software, version 2021, in a multivariate regression analysis of the adapted CCI on the 13 independent potential predictor variables, a simple random sample with N = 553 women (609/1.1) would achieve 96% power to detect an R2 of 0.05 using an F test with an alpha level of 0.05.
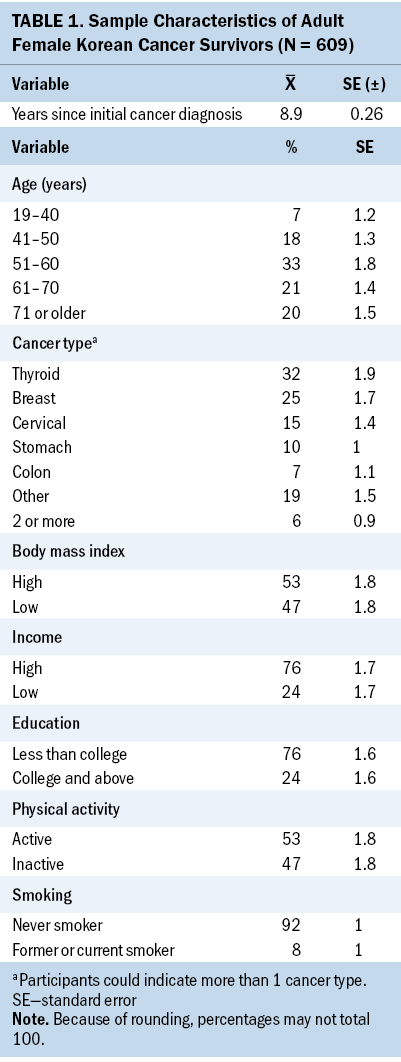
When extrapolated to the adult female Korean population previously diagnosed with cancer, the majority were physically active, were never smokers, had less than a college education, had a high BMI, and had a high income, with an average of 8.9 years since their initial cancer diagnosis (see Table 1).
Bivariate Linear Regression Results
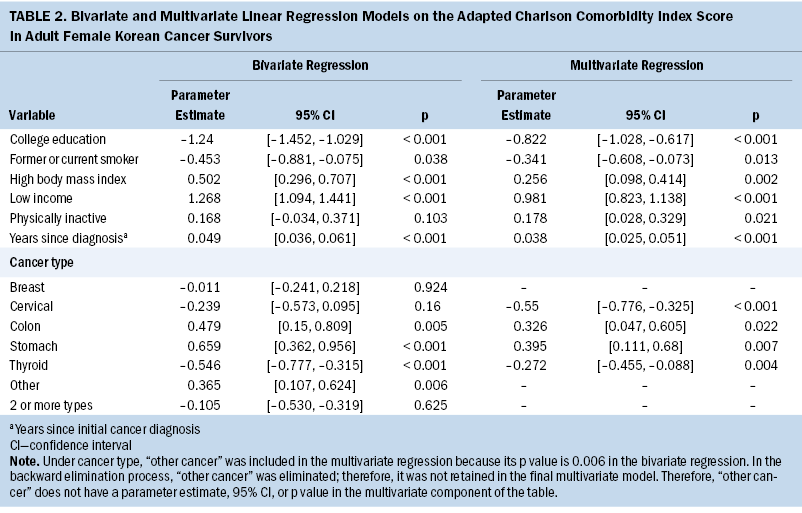
The mean adapted CCI score was 2.4 (SE = 0.052). Bivariate correlation coefficients (Pearson’s r) between all potential predictors of the adapted CCI score were no greater than 0.33, supporting the lack of multicollinearity in the subsequent multivariate regression analysis. In bivariate regression analyses, the following variables were found to be correlated with increased adapted CCI scores (p < 0.2): being diagnosed with stomach cancer; being diagnosed with colon cancer; not being diagnosed with cervical cancer; not being diagnosed with thyroid cancer; being diagnosed with a cancer other than stomach, colon, breast, cervical, or thyroid cancer; having a greater number of years since their initial cancer diagnosis; having a high BMI; being physically inactive; having a low income; not having a college education; and not being a former or current smoker.
Multivariate Linear Regression Results
In multivariate regression analysis, the adapted CCI score significantly increased if diagnosed with stomach cancer, increased if diagnosed with colon cancer, decreased if diagnosed with cervical cancer, decreased if diagnosed with thyroid cancer, increased with a greater number of years since initial cancer diagnosis, increased with a high BMI, increased with physical inactivity, increased with low income, decreased with having a college education, and decreased if a former or current smoker (see Table 2).
Discussion
To the authors’ knowledge, this study is the first to report an analysis of KNHANES data using an adapted version of the CCI to explore factors related to physical comorbidities in adult female Korean cancer survivors.
Analysis of the data found that cancer-related variables (type of cancer and years since initial cancer diagnosis) were related to increased comorbidity. The adapted CCI score was greater in individuals who were diagnosed with stomach and/or colon cancer but lower in individuals diagnosed with cervical or thyroid cancer. These findings are consistent with previous studies from the United States and other countries. A study using data from the New Zealand Cancer Registry found that the prevalence of comorbidities was higher in colorectal and stomach cancers (Sarfati et al., 2016). In addition, in the authors’ previous U.S. study using the National Health and Nutrition Examination Survey, female cancer survivors diagnosed with gynecologic (cervical, ovarian, uterine) cancers had significantly lower CCI scores (Park & Strauss, 2019). In the current study, the adapted CCI score increased with more years since the initial cancer diagnosis. This is consistent with the authors’ previous study of female cancer survivors in the United States (Park & Strauss, 2019) and a previous study using two California cancer registries (Leach et al., 2015). Leach et al. (2015) reported that cancer survivors with more than 10 years since their initial cancer diagnosis were more likely to have comorbidities.
Current findings also indicate that body composition and physical inactivity are important factors associated with higher adapted CCI scores. The adapted CCI score increased with high BMI (overweight and obesity) and physical inactivity. This finding is consistent with the authors’ previous study of female cancer survivors in the United States (Park & Strauss, 2019) and Leach et al.’s (2015) study using two California cancer registries. Among Korean cancer survivors, aerobic physical activity and strength training exercise were related to a lower risk of comorbidities (Kang et al., 2018). However, cancer survivors have increased activity limitations, and no differences were found in physical activity between long-term cancer survivors and the general population (Chun et al., 2015; Oh et al., 2015 ). Most Korean cancer survivors do not meet exercise guidelines, and female cancer survivors have particularly low participation in resistance exercise (Park, Lee, et al., 2021).
Findings from the current study indicated that socioeconomic status may be related to degree of comorbidity. The adapted CCI score increased with lower income but decreased with higher education level, consistent with the authors’ study of adult female cancer survivors in the United States and with those in other countries (Louwman et al., 2010; Mahumud et al., 2020; Park & Strauss, 2019). In particular, among Australian cancer survivors, living in the poorest households was a significant predictor of increased risk for chronic comorbidities (Mahumud et al., 2020). A population-based study in the Netherlands also found that for all of the cancer sites examined, comorbidity prevalence was significantly higher in individuals with newly diagnosed cancer in lower socioeconomic groups (Louwman et al., 2010).
An unexpected finding was that adapted CCI scores decreased if the cancer survivor was a former or current smoker compared to one who never smoked. In the authors’ previous research involving adult female cancer survivors in the United States, 52.1% never smoked, 30.2% were former smokers, and 17.7% were current smokers. In that study, the modified CCI score was lower among current smokers and never smokers than former smokers (Park & Strauss, 2019). This was consistent with the findings of Tammemagi et al. (2004) in their study of the medical records of 1,155 male and female lung cancer survivors. They found that being a former smoker was correlated with having comorbidities, suggesting that former smokers may have needed to quit because of comorbid conditions. In the current study involving adult female cancer survivors in Korea, the authors compared those who never smoked (92.4%) with those who smoked currently or in the past (7.6%). Former smokers may have needed to quit because of comorbid conditions. Regarding current smokers, it is unclear why, when included with former smokers, their CCI score tended to be lower than that of never smokers. Additional research is needed to examine the association between smoking history and the risk of comorbid conditions.
Limitations
The authors acknowledge limitations in the current study. First, most of the data, including those involving cancer and comorbidities, were based on self-report and are therefore subject to possible error or socially desirable responses. Second, many cancer types were grouped as “other cancer,” so not all cancer types could be accounted for in the authors’ analyses. Third, the validity of the adapted CCI used in this study has not been previously examined. Despite these limitations, this study adds to the understanding of adult female Korean cancer survivors, enabling a determination of the correlates of physical comorbidities in this population.
Implications for Nursing and Research
With improved survival, the management of comorbid health conditions has become increasingly important in cancer survivorship care worldwide. Modifiable risk factors such as physical inactivity and obesity are often major causes of chronic disorders as well as cancer recurrence. Timely assessment of and education on modifiable risk factors are critical in cancer survivorship care. However, because of a lack of resources and a lack of acknowledgment of the importance of such care, these risk factors are often unaddressed. Most cancer survivors in Korea report physical, psychological, and socioeconomic problems, but only a small proportion of them receive rehabilitation services regarding their issues (Jo et al., 2010).
A nationwide survey of oncologists and their patients in Korea found that oncologists underestimated the supportive care needs of patients with cancer, and there was a considerable difference in the perception of needed supportive care between oncologists and patients with cancer (Shin et al., 2011). Oncologists reported that lack of knowledge, limited healthcare resources, and lack of established guidelines are major barriers to caring for cancer survivors (Shin, Kim, et al., 2012). In addition, the division of roles and responsibilities between oncologists and primary care providers is not well defined in cancer survivorship care, and preventive measures can often be underemphasized in this care. Oncologists’ confidence in primary care physicians as the main healthcare providers for cancer survivors is low in Korea (Park et al., 2013).
In light of the lack of systematic care for cancer survivors in Korea, there is increased discussion on the optimal care delivery model for cancer survivors (Lim et al., 2018). In a qualitative study performed among healthcare providers, the lack of an interprofessional care system and the absence of a shared care system for long-term survivorship care were identified as limitations to survivorship care in Korea (Lim et al., 2018). An institution-based shared care model where oncologists and primary care physicians collaborate on cancer survivors’ care has been suggested as one of the most feasible options in Korea (Shin et al., 2013). Implementation and subsequent evaluation of such a model is a critical research need.
Nurses and advanced practice nurses among minority populations and in diverse countries, including Korea, are in unique positions to fill the gaps and appropriately educate cancer survivors about risk factors for comorbidities. Findings from the current study can guide the identification of such risk factors in cancer survivors in Korean clinical settings. Beyond the individual level of care, nurses can play a leadership role in cancer survivorship care by disseminating and implementing effective programs in collaboration with the Korean Centers for Disease Control and Prevention (Buchanan et al., 2015; Smith & Hall, 2015). In Korea, model-guided cancer survivorship programs have been tested and found to be effective (Lee et al., 2016). With their clinical assessment as well as community outreach resources and skills, nurses can play a pivotal role in improving cancer survivorship care.
Conclusion
In cancer survivorship care, the management of comorbid health conditions is critical to survival and quality of life. Little is known about the factors related to comorbidities, particularly among minority populations and in countries such as Korea. The current study identified multiple factors related to increased health comorbidities in adult female Korean cancer survivors. Further research is needed to develop systematic cancer survivorship programs to improve the management of health comorbidities in this population.
About the Authors
So-Hyun Park, PhD, APN-BC, RN, is an assistant professor in the Hunter College School of Nursing at the City University of New York in New York; and Shiela M. Strauss, PhD, is a consultant in the Hunter College School of Nursing at the City University of New York and an adjunct professor in the Rory Meyers College of Nursing at New York University in New York. No financial relationships to disclose. Both authors contributed to the conceptualization and design, provided statistical support and the analysis, and contributed to the manuscript preparation. Park can be reached at sp1799@hunter.cuny.edu, with copy to ONFEditor@ons.org. (Submitted November 2021. Accepted May 6, 2022.)
References
Buchanan, N.D., Houston, K.A., & Richardson, L.C. (2015). The essential role of public health in preventing disease, prolonging life, and promoting health of cancer survivors. American Journal of Preventive Medicine, 49(6), S467–S469. https://doi.org/10.1016/j.amepre.2015.08.006
Chan, R.J., Yates, P., Li, Q., Komatsu, H., Lopez, V., Thandar, M., . . . Molassiotis, A. (2017). Oncology practitioners’ perspectives and practice patterns of post-treatment cancer survivorship care in the Asia-Pacific region: Results from the STEP study. BMC Cancer, 17(1), 715. https://doi.org/10.1186/s12885-017-3733-3
Charlson, M.E., Pompei, P., Ales, K.L., & MacKenzie, C.R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Chun, S.Y., Park, H., Lee, T.H., & Park, E. (2015). Do long term cancer survivors have better health-promoting behavior than non-cancer populations?: Case-control study in Korea. Asian Pacific Journal of Cancer Prevention, 16(4), 1415–1420. https://doi.org/10.7314/APJCP.2015.16.4.1415
Deimling, G.T., Sterns, S., Bowman, K.F., & Kahana, B. (2005). The health of older-adult, long-term cancer survivors. Cancer Nursing, 28(6), 415–424. https://doi.org/10.1097/00002820-200511000-00002
Hwang, S.M., Yoon, S.J., Ahn, H.S., An, H.G., Kim, S.H., Kyeong, M.H., & Lee, E.K. (2009). Usefulness of comorbidity indices in operative gastric cancer cases. Journal of Preventive Medicine and Public Health, 42(1), 49–58. https://doi.org/10.3961/jpmph.2009.42.1.49
Hwangbo, Y., Kang, D., Kang, M., Kim, S., Lee, E.K., Kim, Y.A., . . . Cho, J. (2018). Incidence of diabetes after cancer development: A Korean national cohort study. JAMA Oncology, 4(8), 1099–1105. https://doi.org/10.1001/jamaoncol.2018.1684
Jang, M.K., Kim, S., Park, C.G., Collins, E.G., Quinn, L.T., & Ferrans, C.E. (2020). Quality of life and prolonged symptoms in Korean breast cancer survivors. Cancer Nursing, 45(1), E124–E133. https://doi.org/10.1097/NCC.0000000000000894
Jo, J.M., Hwang, J.H., Lee, C.H., Kang, H.J., & Yu, J.N. (2010). The need of cancer patients for rehabilitation services. Journal of Korean Academy of Rehabilitation Medicine, 34(6), 691–700.
Jung, K.W., Won, Y.J., Kong, H.J., & Lee, E.S. (2019). Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2016. Cancer Research and Treatment, 51(2), 417–430. https://doi.org/10.4143/crt.2019.138
Kang, D., Lee, E., An, K.Y., Min, J., Jeon, J.Y., & Courneya, K.S. (2018). Associations between physical activity and comorbidities in Korean cancer survivors. Journal of Cancer Survivorship, 12(4), 441–449. https://doi.org/10.1007/s11764-018-0683-y
Kim, Y. (2014). The Korea National Health and Nutrition Examination Survey (KNHANES): Current status and challenges. Epidemiology and Health, 36, e2014002. https://doi.org/10.4178/epih/e2014002
Koh, D., Song, S., Moon, S.E., Jung, S.Y., Lee, E.S., Kim, Z., . . . Lee, J.E. (2019). Adherence to the American Cancer Society guidelines for cancer survivors and health related quality of life among breast cancer survivors. Nutrients, 11(12), 2924. https://doi.org/10.3390/nu11122924
Korea Disease Control and Prevention Agency. (n.d.). Korea National Health and Nutrition Examination Survey. https://knhanes.kdca.go.kr/knhanes/main.do
Korea Disease Control and Prevention Agency. (2019). Data analysis guidelines. https://knhanes.kdca.go.kr/knhanes/sub03/sub03_06_02.do
Kweon, S., Kim, Y., Jang, M.J., Kim, Y., Kim, K., Choi, S., . . . Oh, K. (2014). Data resource profile: The Korea National Health and Nutrition Examination Survey. International Journal of Epidemiology, 43(1), 69–77. https://doi.org/10.1093/ije/dyt228
Leach, C.R., Weaver, K.E., Aziz, N.M., Alfano, C.M., Bellizzi, K.M., Kent, E.E., . . . Rowland, J.H. (2015). The complex health profile of long-term cancer survivors: Prevalence and predictors of comorbid conditions. Journal of Cancer Survivorship, 9(2), 239–251. https://doi.org/10.1007/s11764-014-0403-1
Lee, J.E., Shin, D.W., Lee, H., Son, K.Y., Kim, W.J., Suh, Y.S., . . . Yang, H.K. (2016). One-year experience managing a cancer survivorship clinic using a shared-care model for gastric cancer survivors in Korea. Journal of Korean Medical Science, 31(6), 859–865. https://doi.org/10.3346/jkms.2016.31.6.859
Lee, J.Y., Lee, D.H., Cho, N.H., Rha, K.H., Coi, Y.D., Hong, S.J., . . . Cho, K.S. (2014). Impact of Charlson Comorbidity Index varies by age in patients with prostate cancer treated by radical prostatectomy: A competing risk regression analysis. Annals of Surgical Oncology, 21(2), 677–683. https://doi.org/10.1245/s10434-013-3326-6
Lim, J.W., Shon, E.J., & Yang, E.J. (2018). A qualitative study of healthcare providers’ perceptions and suggestions for developing cancer survivorship care models in South Korea. European Journal of Cancer Care, 27(1), e12613. https://doi.org/10.1111/ecc.12613
Louwman, W.J., Aarts, M.J., Houterman, S., van Lenthe, F.J., Coebergh, J.W.W., & Janssen-Heijnen, M.L.G. (2010). A 50% higher prevalence of life-shortening chronic conditions among cancer patients with low socioeconomic status. British Journal of Cancer, 103(11), 1742–1748. https://doi.org/10.1038/sj.bjc.6605949
Mahumud, R.A., Alam, K., Dunn, J., & Gow, J. (2020). The burden of chronic diseases among Australian cancer patients: Evidence from a longitudinal exploration, 2007-2017. PLOS ONE, 15(2), e0228744. https://doi.org/http://dx.doi.org/10.1371/journal.pone.0228744
Mickey, R.M., & Greenland, S. (1989). The impact of confounder selection criteria on effect estimation. American Journal of Epidemiology, 129(1), 125–137. https://doi.org/10.1093/oxfordjournals.aje.a115101
Noh, H.M., Park, Y.S., Lee, H.J., Roh, Y.K., & Song, H.J. (2019). Association between sodium density and grip strength among older Korean adults: A nationwide cross-sectional study. Clinical Interventions in Aging, 14, 2163–2171. https://doi.org/10.2147/cia.s228290
Oh, C., Lee, D., Kong, H., Lee, S., Won, Y., Jung, K., & Cho, H. (2020). Causes of death among cancer patients in the era of cancer survivorship in Korea: Attention to the suicide and cardiovascular mortality. Cancer Medicine, 9(5), 1741–1752. https://doi.org/10.1002/cam4.2813
Oh, M.G., Han, M.A., Byeon, Y.M., Bae, K.M., & Choi, S. (2015). Assessing activity limitation among cancer survivors in Korea using data from a nationwide survey. Asian Pacific Journal of Cancer Prevention, 16(7), 2739–2743. https://doi.org/10.7314/APJCP.2015.16.7.2739
Park, C.H., Kim, Y., Mo, H.N., Kong, K.A., Choi, J.Y., Jho, H.J., & Uem, T.S. (2013). Oncologist’s expectations on primary physician for sharing care of cancer survivor in Korea. Korean Journal of Family Practice, 3(2), 168–176.
Park, J., Han, K., Shin, D.W., Park, S.H., & Shin, H.B. (2021). Conditional relative survival and competing mortality of patients with prostate cancer in Korea: A nationwide cohort study. Cancer Epidemiology, Biomarkers and Prevention, 30(2), 326–334. https://doi.org/10.1158/1055-9965.EPI-20-1084
Park, J.H., Lee, J.S., Ko, Y.H., & Kim, Y.H. (2021). Physical activity of Korean cancer survivors is associated with age and sex. Korean Journal of Internal Medicine, 36(Suppl. 1), S225–S234. https://doi.org/10.3904/kjim.2019.240
Park, S.H., & Strauss, S.M. (2019). Similarities and differences in the correlates of comorbidities in U.S. male and female adult cancer survivors. Public Health Nursing, 36(4), 478–487. https://doi.org/10.1111/phn.12617
Porta, M.S. (Ed.). (2014). A dictionary of epidemiology (5th ed.). Oxford University Press.
Quan, H., Li, B., Couris, C.M., Fushimi, K., Graham, P., Hider, P., . . . Sundararajan, V. (2011). Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. American Journal of Epidemiology, 173(6), 676–682. https://doi.org/10.1093/aje/kwq433
Rock, C.L., Thomson, C., Gansler, T., Gapstur, S.M., McCullough, M.L., Patel, A.V., . . . Doyle, C. (2020). American Cancer Society guideline for diet and physical activity for cancer prevention. CA: A Cancer Journal for Clinicians, 70(4), 245–271. https://doi.org/10.3322/caac.21591
Sarfati, D., Gurney, J., Lim, B.T., Bagheri, N., Simpson, A., Koea, J., & Dennett, E. (2016). Identifying important comorbidity among cancer populations using administrative data: Prevalence and impact on survival. Asia-Pacific Journal of Clinical Oncology, 12(1), e47–e56. https://doi.org/10.1111/ajco.12130
Sarfati, D., Tan, L., Blakely, T., & Pearce, N. (2011). Comorbidity among patients with colon cancer in New Zealand. New Zealand Medical Journal, 124(1338), 76–88.
Shackman, G. (2001, March 24). Sample size and design effect [Presentation]. Albany Chapter of American Statistical Association, United States.
Shin, D.W., Ahn, E., Kim, H., Park, S., Kim, Y.A., & Yun, Y.H. (2010). Non-cancer mortality among long-term survivors of adult cancer in Korea: National cancer registry study. Cancer Causes and Control, 21(6), 919–929. https://doi.org/10.1007/s10552-010-9521-x
Shin, D.W., Cho, B., Kim, S.Y., Jung, J.H., & Park, J.H. (2013). Management of cancer survivors in clinical and public health perspectives: Current status and future challenges in Korea. Journal of Korean Medical Science, 28(5), 651–657. https://doi.org/10.3346/jkms.2013.28.5.651
Shin, D.W., Kim, Y., Baek, Y., Mo, H., Choi, J., & Cho, J. (2012). Oncologists experience with second primary cancer screening: Current practices and barriers and potential solutions. Asian Pacific Journal of Cancer Prevention, 13(2), 671–676. https://doi.org/10.7314/apjcp.2012.13.2.671
Shin, D.W., Kim, S.Y., Cho, J., Sanson-Fisher, R.W., Guallar, E., Chai, G.Y., . . . Park, J. (2011). Discordance in perceived needs between patients and physicians in oncology practice: A nationwide survey in Korea. Journal of Clinical Oncology, 29(33), 4424–4429. https://doi.org/10.1200/jco.2011.35.9281
Shin, D.W., Park, J.H., Park, J.H., Park, E.C., Kim, S.Y., Kim, S.G., & Choi, J.Y. (2010). Antihypertensive medication adherence in cancer survivors and its affecting factors: Results of a Korean population-based study. Supportive Care in Cancer, 19(2), 211–220. https://doi.org/10.1007/s00520-009-0802-4
Shin, D.W., Park, J.H., Shim, E., Hahm, M., Park, J., & Park, E. (2012). Predictors and outcomes of feeling of insufficient consultation time in cancer care in Korea: Results of a nationwide multicenter survey. Supportive Care in Cancer, 20(9), 1965–1973. https://doi.org/10.1007/s00520-011-1299-1
Shin, J., Shim, H.Y., & Jun, J.K. (2014). Comparison of diabetes management status between cancer survivors and the general population: Results from a Korean population-based survey. PLOS ONE, 9(10), e110412. https://doi.org/10.1371/journal.pone.0110412
Shin, J., Shin, D.W., Lee, J., Hwang, J., Yoo, J.E., Ko, H., & Song, Y. (2020). Association between perception of care coordination and health outcomes in Korean cancer survivors. Health and Quality of Life Outcomes, 18(1), 21. https://doi.org/10.1186/s12955-020-1279-6
Smith, J.L., & Hall, I.J. (2015). Advancing health equity in cancer survivorship. American Journal of Preventive Medicine, 49(6), S477–S482. https://doi.org/10.1016/j.amepre.2015.08.008
Tammemagi, C.M., Neslund-Dudas, C., Simoff, M., & Kvale, P. (2004). In lung cancer patients, age, race-ethnicity, gender and smoking predict adverse comorbidity, which in turn predicts treatment and survival. Journal of Clinical Epidemiology, 57(6), 597–609. https://doi.org/10.1016/j.jclinepi.2003.11.002
Wen, K., Fang, C.Y., & Ma, G.X. (2014). Breast cancer experience and survivorship among Asian Americans: A systematic review. Journal of Cancer Survivorship, 8(1), 94–107. https://doi.org/10.1007/s11764-013-0320-8
West, B.T., Sakshaug, J.W., & Aurelien, G.A.S. (2018). Accounting for complex sampling in survey estimation: A review of current software tools. Journal of Official Statistics, 34(3), 721–752. https://doi.org/10.2478/jos-2018-0034
Woo, H.K., Park, J.H., Kang, H.S., Kim, S.Y., Lee, S.I., & Nam, H.H. (2010). Charlson Comorbidity Index as a predictor of long-term survival after surgery for breast cancer: A nationwide retrospective cohort study in South Korea. Journal of Breast Cancer, 13(4), 409. https://doi.org/10.4048/jbc.2010.13.4.409
World Health Organization Expert Consultation. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403), 157–163. https://doi.org/10.1016/s0140-6736(03)15268-3
Yang, E.J., Chung, S.H., Jeon, J., Seo, K.S., Shin, H., Hwang, J.H., & Lim, J. (2015). Current practice and barriers in cancer rehabilitation: Perspectives of Korean physiatrists. Cancer Research and Treatment, 47(3), 370–378. https://doi.org/10.4143/crt.2014.084


