Engaging Older Adults With Cancer and Their Caregivers to Set Research Priorities Through Cancer and Aging Research Discussion Sessions
Purpose: To report on the perspectives of older adults (aged older than 65 years) with cancer and their caregivers who participated in patient-oriented research priority–setting activities called the Cancer and Aging Research Discussion Sessions.
Participants & Setting: 35 older adults and caregivers participated in three public meetings and follow-up interviews.
Methodologic Approach: Qualitative descriptive.
Findings: There was clear consensus from participants on research priorities related to two key areas: enhanced communication and tailored cancer support for older adults, encompassing the following five research priorities: (a) improved patient–provider communication, (b) technology-based solutions, (c) desire for enhanced patient education strategies addressing multimorbidity and aging-sensitive needs, (d) tangible and accessible survivorship supports, and (e) support for caregivers and caregiver needs.
Implications for Nursing: Future research should focus on addressing age-related disparities in cancer care communication and support. By capitalizing on older adults’ interest in research engagement, effective solutions can be cocreated to improve cancer experiences for older adults and their caregivers.
Jump to a section
Cancer is common among older adults globally, and the numbers are expected to increase in incidence, ranging from 54% in more developed regions to 144% in less developed regions by 2035 (Pilleron et al., 2019). This increasing incidence matters because older adults with cancer have age-related needs, which, if left unmet, may lead to health disparities, including the deleterious impacts of over- and undertreatment (DuMontier et al., 2020). These unique needs of older adults include demands of multimorbidity (Sarfati et al., 2016), potentially high symptom burden, and susceptibility to treatment toxicities (Nipp et al., 2016). In addition, the physical consequences of cancer, alongside psychosocial consequences, such as emotional distress and memory changes, may be more burdensome for older adults experiencing comorbid conditions, frailty, and functional decline (Pal et al., 2010; Schouten et al., 2019). Transition from treatment to survivorship or post-treatment can be equally challenging given the complex management of existing chronic conditions and potential accumulation of new comorbidities resultant of treatment (Leach et al., 2015; Tolbert et al., 2018).
For older adults, a cancer diagnosis also affects caregivers, and prior research demonstrates the criticality of caregivers in supporting older adults with cancer (Hsu et al., 2014; Kent et al., 2016; Tolbert et al., 2018). Given the prevalence of functional decline among older adults with cancer (Amemiya et al., 2007; Hurria et al., 2019; Kenis et al., 2017), caregivers are a key support for getting patients to and from treatment and supporting symptom management in the intervening period (Hsu et al., 2014; PDQ Supportive and Palliative Care Editorial Board, 2010).
Recent and growing efforts to engage people with lived experience (often characterized as patients) in designing and conducting research are occurring globally (Gilmore et al., 2019; Puts, Sattar, Ghodraty-Jabloo, et al., 2017; Sacristán, 2013). Patient-oriented, patient-engaged, and patient and public involvement in research involves people with current or past illness experience in setting research priorities, conducting research, analyzing, and translating data (Chudyk et al., 2018; Pii et al., 2019). The levels of patient involvement in research have also been categorized across a spectrum ranging from informing and consulting (low end of engagement) to participation, consultation, involvement, collaboration, and leading (the highest level of engagement) (Amirav et al., 2017; Boivin et al., 2018). The ultimate goal of patient-oriented research is to shape health research by shifting the role of patients from passive receptors of research and services to proactive partners sharing their lived experience in shaping the research process (Canadian Institutes of Health Research, 2015).
Given the aging population and increasing numbers of older adults diagnosed and living with cancer, it is important to understand research priorities related to optimizing cancer care from the perspectives of older adults with cancer and their caregivers. The purpose of this article is to report findings from public meetings and follow-up interviews where older adults with cancer and their caregivers participated in research priority–setting sessions. The research questions were as follows:
• What are the research priorities of older adults with cancer and their caregivers?
• What are older adults’ and their caregivers’ perspectives on future engagement in research?
Methods
The authors used a qualitative descriptive approach to understand patient and caregiver perspectives of research priorities to enhance care based on their experiences with cancer and their perspectives on engagement in research (Colorafi & Evans, 2016; Sandelowski, 2000). The authors operationalized patient involvement in this project at multiple levels by involving a patient as co-lead and author on this project (M.A.T.) and by consulting and engaging patients in the priority-setting sessions and interviews (Boivin et al., 2018). Ethical approval was sought and received from the University of Saskatchewan Research Ethics Board. The authors received an ethics exemption for the initial priority-setting sessions and full approval for the follow-up interviews. All participants in the interviews completed a consent form.
Sample and Setting
The authors worked with local cancer support groups and the local cancer agency to advertise the priority-setting sessions by placing posters in the cancer clinic and disseminating the poster via support group social media pages. The authors sought adults aged 65 years or older who had received a diagnosis of cancer and had undergone (or were currently receiving) treatment for cancer and anyone who identified as a caregiver of an older adult with cancer. Caregivers and older adults did not have to participate as a dyad; for example, a caregiver could participate without the person for whom they cared. All sessions were held in person; to facilitate involvement, the authors provided transportation support in the form of taxi reimbursement and held sessions in wheelchair-accessible community locations with free parking. Refreshments were provided to create a warm and welcoming environment. Priority-setting sessions were held in two major cities within the province, Saskatoon and Regina, that serve northern and southern residents, respectively. Sample size in qualitative research is a matter of feasibility, judgment, and population access (Sandelowski, 1995; Sim et al., 2018), and the authors planned to conduct two focus groups based on the expectation that cancer care priorities would be similar among participants. Despite seeing repetition in themes after the first two focus groups, the authors decided to conduct one more focus group to ensure that there were no outstanding priorities.
Follow-up interviews took place via telephone, thereby mitigating factors related to transportation for older adults and their caregivers. Telephone interviews enabled participants from rural communities to participate in interviews without traveling great distances.
Procedures
Participants interested in priority-setting sessions contacted the lead author (K.R.H.) to indicate interest and availability and were given information about the session. On the day of the session, participants were given a folder with documents describing the plan for the session, as well as an evaluation form. The large group was divided into smaller groups (six people per group), each with a facilitator and a note taker. The small groups then reconvened as one large group to share their findings. The authors structured the discussion groups around challenges and opportunities in the cancer trajectory (diagnosis, treatment, and survivorship). Following the session, participants completed an evaluation of their involvement and interest in future research and indicated their interest in participating in follow-up interviews. Participants who indicated an interest in interviews were contacted by telephone by a research assistant. Interview guides were developed based on discussion and feedback on evaluation forms from the in-person sessions, including research priorities and preferences for future research involvement (see Figure 1). 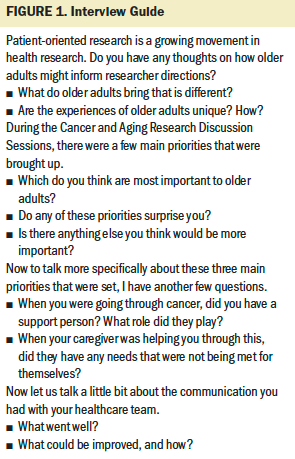
Analysis
The authors used thematic analysis to assess and describe patterned meaning in the data (Braun et al., 2019). Data analysis was conducted by K.R.H. and S.S. using NVivo coding software and Microsoft® Excel®. First, evaluations from the discussion sessions were collated in Microsoft Excel; numeric data were analyzed using descriptive statistics (means and frequencies). Session notes were assigned a descriptive label and then grouped by broader themes. Interview transcripts were read line by line and reviewed for salient themes by generating initial codes and subsequently grouping into larger themes. The patient coauthor (M.A.T.) was involved in the initial analysis by reviewing the framework and interpretations and sharing her perceptions, which were used to modify the framework and inform future analysis. Analysis was considered complete when all authors agreed on the framework. The last step of analysis involved triangulation and integration of all data sources (session evaluations, facilitator notes, and interview data) to fully describe participants’ views. The authors established trustworthiness and rigor in this study using the principles of credibility, transferability, dependability, and confirmability (Lincoln & Guba, 1985). The authors did so by engaging in analyses for a prolonged period of time, engaging multiple parties with multiple positions and identities in data analysis, triangulating multiple data sources, and having a patient partner as coauthor to validate the interpretations.
Findings
Three priority-setting sessions took place between June and September 2019 in two urban centers in the Canadian province of Saskatchewan, with participants attending from rural and urban areas. A total of 35 older adults with cancer and those who identified as caregivers participated in these community discussion sessions, which lasted from three to four hours per session. Some participants were still receiving cancer treatment, whereas others had recently completed treatment. Caregiving experience varied from those recently bereaved and those still engaged in caring work. The majority of participants were female (71%), and a range of cancer types was represented (see Table 1). Participants identified as patients (n = 25), caregivers (n = 8), or both (n = 2). For most (n = 27), this was their first exposure to and participation in research, either as a participant in a research study or as a consultant on research priority setting. Participants were asked to rank their enjoyment of the session on a five-point scale ranging from 1 (very negative) to 5 (very positive), with an average score of 4. Eleven individuals from the focus groups participated in follow-up interviews. The authors will discuss the five research priorities (research question 1), followed by future engagement in research (research question 2). 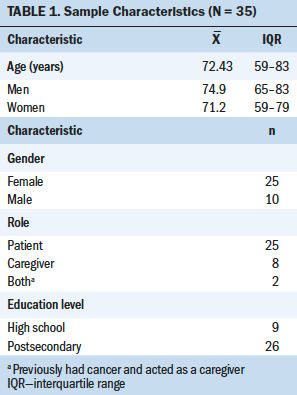
Based on the analysis of interactions with participants during the focus groups and interviews, the authors identified the following five research priorities: (a) improved patient–provider communication, (b) technology-based solutions, (c) desire for enhanced patient education strategies addressing multimorbidity and aging-sensitive needs, (d) tangible and accessible survivorship supports, and (e) support for caregivers and caregiver needs (see Figure 2). The authors organized these into two main themes related to communication (priorities 1 and 2) and tailored cancer support for older adults (priorities 3–5). 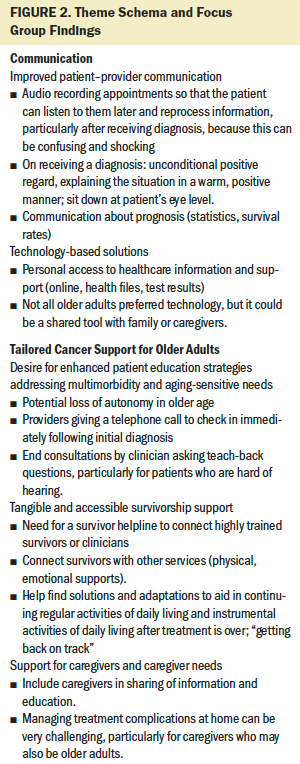
Research Priorities Related to Communication
Across the cancer trajectory, older adult and caregiver participants found that communication was a key area that required further research and support. The reflections on communication related to interpersonal communication among participants, caregivers, and clinicians. Not all experiences were bad; therefore, there was consideration among participants about what traits made communication and cancer experiences “good” and what could make them better. Participants also discussed the present and growing role of technology in cancer treatment and survivorship and presented solutions that could be a focus of future research.
Improved patient–provider communication (research priority 1): Some older adults described feeling very challenged around the time of diagnosis. Those who had positive experiences described a situation where they were told about their diagnosis in a warm and positive manner and their clinician was able to speak to them loudly and slowly in a way that they could hear and understand.
Many older adults described that communication among the patient, caregiver, and provider could have been improved, feeling as follows: “We didn’t really have a cohesive continuity of care.” This was amplified by the fact that most older adults had existing chronic conditions and saw multiple specialists, which contributed to the discontinuity. Although many participants lauded the care they received (for example, by stating it was “very matter of fact and kind”), some described receiving “zero support.” Frequently, older adults described not remembering what was said at diagnosis and treatment consultations. This was particularly important for older adults who described having memory problems, or for those who were unable to bring a caregiver with them and attended these meetings alone. One participant stated the following:
I had my husband with me to think of things that I didn’t think of, so we had that opportunity . . . but not everybody has somebody to go with them. Sometimes people are there on their own, or maybe just somebody driving them there and picking them up.
The idea of a written record of all appointments—written at a comprehendible, jargon-free level—was a suggestion on which most participants agreed. This written record was seen as a way to connect older adults with their providers and provide a simple vehicle for information that could be shared with caregivers. This written record was also seen as a way to share the information with primary care and specialist physicians, which was a concern given that most older adults had more than one chronic illness. Participants also suggested the idea of bringing a voice recorder to appointments so that they could listen to it later and process the information.
Technology-based solutions (research priority 2): Although communication was seen as an opportunity to improve the patient experience, the use of technology was another potential area of discussion. Most participants made use of the telephone during cancer treatment and survivorship. However, participants acknowledged that they (and their families) searched the internet for information and used discussion boards to find information about cancer and see the stories of people with a similar diagnosis. Although participants had varying levels of interest in eHealth interventions (ranging from not at all to very interested), there was general consensus that these types of support could enhance the care experience for most older adults and their caregivers. Some felt that just because they were older adults and may not be as interested in using specific types of technology, it did not mean that they (or their family members) could not benefit from having it. These types of resources were seen as particularly useful for those who had multiple comorbidities and sought ways to organize all their care. Older adults also referenced the importance of having personal access to healthcare information, support, and health records, further reinforcing the need for some form of written record and describing an interest in “access to healthcare information online.”
Research Priorities Related to Tailored Cancer Support for Older Adults
Many older adults related their experiences with cancer around their perspective as older adults, saying things like, “I’ve had a good life,” and describing older adults as “a person who is past the age of 65, and basically has lived their life.” In this way, older adults contextualized their cancer experiences within lives lived. However, they also emphasized the importance of considering what they felt were their many unmet needs because they were older, which related directly to aging and living in an “old” body. They referenced the importance of patient education strategies that addressed their coexisting chronic diseases during active cancer treatment, the need for resources that consider these needs in the survivorship period, and support for their caregivers.
Desire for enhanced patient education strategies addressing multimorbidity and aging-sensitive needs (research priority 3): Participants described that by being older and having cancer, they may be perceived as having less autonomy related to treatment decision-making. They felt that they would benefit from things like a telephone call from their clinician to check on them immediately after their diagnosis to make sure that they heard what was discussed during the session. Multimorbidity was a common concern, and the notion of a written record was seen as a way to align multiple healthcare providers. For example, one participant described how he had multiple chronic conditions and he was not sure who was caring for what, which led to him missing his treatments, as follows:
The cancer clinic said afterwards that they thought my GP [general practitioner] was doing it, and my GP said, “No, I thought the cancer clinic was doing it,” so I missed chemo[therapy] treatments because of complications from being on too much blood thinners for my weight.
Many participants also experienced vision loss, mobility challenges, and other age-related concerns and needed extra support, which was not readily provided. There was a feeling that support should be provided without having to ask for it, because many participants felt uncomfortable asking. Many older adults felt that they would not ask for those supports, such as a social worker, but when they reflected on their experience and heard of others in the focus groups who had this support, they felt they really could have used it. One participant stated the following:
What always scares me is the people who have nobody to speak up for them. And I’m afraid I see this in nursing homes and in a lot of places, that people don’t have anybody to advocate for them.
Tangible and accessible survivorship supports (research priority 4): Older adults felt that their concerns around cancer extended into the survivorship period, feeling that they needed additional resources in the survivorship phase, particularly related to “getting back on track.” Older adults and caregivers described a disconnect between primary and specialist care when discharged from cancer care and described that they “felt alone.” Participants felt that the follow-up with primary care was challenging because they said, “‘Come whenever you feel like it.’ Therefore, ownership is placed on [the] patient and they may not understand when to seek more help.” Some older adults felt that a connection with fellow older adult cancer survivors would have given a psychological and emotional boost. Participants also felt that new comorbidities that developed as a result of cancer treatment (on top of existing comorbidities accumulated with age) were not well presented at the time of treatment decision-making. As survivors (which was the preferred term of participants), older adults felt unsupported in managing these new conditions.
Support for caregivers and caregiver needs (research priority 5): Finally, many participants acknowledged that their caregivers were also older adults who played a critical role in their care. From the focus groups, one woman who had an older adult caregiver stated the following: “There was always two of us. Some of them had nobody as a caregiver, nothing to fall back on.” Another woman stated the following:
My husband went with me to all my appointments, and he went and sat beside me when I had chemo[therapy] and sat in the waiting room when I [had] radiation. And I think the role of caregivers is critical. I wouldn’t have wanted to go through this without my husband.
Some of the challenges that were presented about caregivers included not receiving adequate information and not being involved in the care process. Older adults and their caregivers felt that managing treatment symptoms and complications was very challenging, particularly for caregivers who were themselves older. One woman described that as she was receiving treatment, her caregiver (also aged older than 80 years) would fall asleep in his car outside. He would then be required to drive her home after hours-long treatment sessions. She was not aware that there were services available to support her.
Engagement in Research
The majority of participants had not taken part in a research priority–setting activity in the past, and most found that the session was a good use of time. Eight older adults had taken part in research studies as participants (e.g., clinical trials, exercise interventions) on topics related to cancer, mobility, and dementia. However, no participants had participated as patient partners on the research team or priority-setting processes. Participants appreciated that they could share their experiences in a group session, with minimal expectation for future involvement. Of all the session participants, three-fourths (n = 27) were interested in future involvement in research projects. Participants told the authors that they appreciated the opportunity to participate in short-term or one-time research opportunities, but most did not want sustained involvement in long-term research activities. This was particularly true for older adults who were concerned about cancer recurrence or had an uncertain prognosis. Caregivers who were recently bereaved were not interested in sustained research involvement.
Discussion
Through the authors’ research priority–setting sessions and interviews with older adults and caregivers, they identified gaps in care delivery through the treatment and survivorship period and the demands placed on their (often) aging caregivers. The main priorities related to enhanced communication and tailored cancer support for older adults. Older adults described being willing, able, and enthusiastic about participating in research opportunities and expressed interest in future participation in research projects as coresearchers.
All the priorities identified by the participants emphasized the need for age-friendly approaches to cancer care related to communication and education (e.g., education strategies that allowed for increased time for participants to process and understand information because of hearing or cognitive challenges). Research also shows that existing interventions that support older adult patients receiving treatment for cancer often do not target complex issues, such as impact of geriatric syndromes (e.g., multimorbidity, frailty) (Farrington et al., 2019). These priorities for age-friendly education have previously been identified (Bourbonniere & Kagan, 2004) and require considerations in domains of knowledge, attitudes, and skills (Hsu, 2016; Odegard et al., 2007). The authors’ findings related to priorities identified by older adults with cancer were similar to those identified by Puts, Sattar, Fossat, et al. (2017), who brought together older adults with cancer and caregivers (n = 52) in an urban center in Canada and found the need for improved patient–provider relationships and caregiver support, and a desire for technology-focused interventions to facilitate the management of their cancer-related needs. The confirmation of these needs within a sample that is reflective of an urban and rural population, in a project co-led with a patient partner, indicates that these are cross-cutting concerns that need to be addressed.
Post-treatment survivorship and caregiver support were identified as important priorities for participants. Again, these challenges included communication and the importance of catering to impairments when distributing written material and conducting verbal conversations, which have been described elsewhere (Mohile et al., 2020). The importance of considerations related to managing existing and new morbidities (arising from cancer treatment) was also emphasized. These findings suggest that more work is required in the area of survivorship among older adults with cancer to target and support their unique needs. The need for attention to caregivers in the context of older adults living with cancer (particularly because they themselves may be older adults), was highlighted by numerous participants and has been mentioned in prior research (Kadambi et al., 2020). The importance of these concerns has been described previously (PDQ Supportive and Palliative Care Editorial Board, 2010), and the current findings confirm that intervention to support this growing population of older adults is required.
An interesting finding from the sessions relates to the desire by some participants for resources that are web-based and accessible by their smartphone or computer. This represents a growing uptake of technology by the population aged 65 years or older that has seen a rapid acceleration, particularly in light of the COVID-19 pandemic (Hollander & Carr, 2020; Ueda et al., 2020). Given the geography in Canada, access to online interventions could do well to mitigate limitations in access to resources for those living in rural and remote regions. However, due attention must be paid in future intervention development to not exclude those who may most need these interventions but are unable or unwilling to use technology (Haight et al., 2014; Hall et al., 2015).
The authors found that most older adults in the sample were interested in participating in future research; however, most preferred shorter, time-limited commitments rather than sustained involvement in research projects. This is an important methodologic finding for those interested in conducting patient-engaged or patient-oriented research with this population, and researchers must be ready to identify opportunities to participate in research activities that account for this preference. This has been described and articulated in numerous ways, but generally research involvement has been characterized across a spectrum from low involvement (consultant roles) to highly engaged roles (coauthors or co-leads who received training for their participation) (Amirav et al., 2017; Vandall-Walker, 2017). For future research with older adults, time frame and expectations of involvement are important considerations.
Limitations
The current study had a small number of participants consistent with the in-depth qualitative research approach. The methods of advertisement for the study, the location of the community groups, and accessibility issues of potential participants may have limited those who participated. Those who chose to participate may have been more interested in research and motivated to seek information, more literate, and more likely to be comfortable with technology. The authors did not collect data on time since cancer diagnosis or caregiving experience, or why individuals chose not to take part in the interview. A strength of this study was that participants came from two urban centers, with some participants traveling from rural areas to attend meetings, thereby representing a more diverse cross-section of viewpoints.
Implications for Nursing
Older adults with cancer and their caregivers who participated in these community sessions expressed several challenges when receiving care at different points in the cancer trajectory. The identified priorities provide a road map for research and oncology nursing to improve care for older adults and their caregivers. The priorities the authors identified have implications for practice and how support is provided for older adults with cancer. For example, an important implication for oncology nursing practice relates to training and education of oncology staff to increase their awareness and knowledge of special considerations that need attention when working with or communicating with older adults. A survey informing an international position statement from the International Society of Geriatric Oncology, European Oncology Nursing Society, and Canadian Association of Nurses in Oncology (and endorsed by the Oncology Nursing Society) documents that nurses understand that older adults with cancer have many unmet needs but feel ill equipped to address them (Puts et al., 2021). Specific suggestions to increase nurses’ knowledge include attending workshops to enhance their knowledge or obtaining certification in geriatric specialization (e.g., the Geriatric Oncology Workshop developed at City of Hope [Burhenn et al., 2020]). Future research related to knowledge translation strategies to enhance care for older adults will be critical to addressing and intervening to support older adults’ needs. 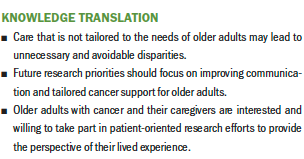
Conclusion
Older adults with cancer and their caregivers expressed unique perspectives on participating in research. By capitalizing on older adults’ interest in research engagement, effective solutions can be cocreated to improve the patient experience. The authors’ findings demonstrate that it is critical to offer older adults a range of involvement in research activities. Such strategies will allow older adults to share their patient experience without overburdening them with unrealistic expectations.
About the Author(s)
Kristen R. Haase, RN, PhD, is an assistant professor in the School of Nursing at the University of British Columbia in Vancouver; Margaret A. Tompson, MCEd, PhD, FCAOT, is a patient representative at Saskatchewan Centre for Patient-Oriented Research in Saskatoon; Steven Hall, BScN, is an RN and a master of nursing student in the College of Nursing at the University of Saskatchewan in Saskatoon; Schroder Sattar, RN, PhD, is an assistant professor in the College of Nursing at the University of Saskatchewan; and Shahid Ahmed, MD, PhD, is a professor in the Division of Oncology in the College of Medicine and a medical oncologist at Saskatchewan Cancer Agency, both at the University of Saskatchewan, all in Canada. Haase and Tompson are dual first authors. No financial relationships to disclose. Haase, Sattar, and Ahmed contributed to the conceptualization and design. Haase, Tompson, Hall, and Sattar completed the data collection. Haase provided statistical support. Haase, Hall, and Sattar provided the analysis. Haase, Tompson, Hall, and Ahmed contributed to the manuscript preparation. Haase can be reached at kristen.haase@ubc.ca, with copy to ONFEditor@ons.org. (Submitted March 2021. Accepted May 13, 2021.)

