Perceived Quality of Work Life and Risk for Compassion Fatigue Among Oncology Nurses: A Mixed-Methods Study
Purpose/Objectives: To examine factors that influenced the nurse’s perceived quality of work life and risk for compassion fatigue (CF). The specific aims of the study were to describe the (a) relationship among nurse characteristics and perceived quality of work life, (b) relationship between personal life stress and perceived quality of work life, and (c) the nurse’s beliefs about his or her risk for CF.
Research Approach: A descriptive, mixed-methods study.
Setting: A hematology-oncology unit in a large urban teaching hospital in Pennsylvania.
Participants: 20 oncology nurses.
Methodologic Approach: Descriptive study using questionnaires and in-depth interviews. The variables were nurse characteristics, personal life stress, and quality of work life. Data were analyzed descriptively and thematically. Scores on the self-report questionnaires were compared to themes.
Findings: Personal life stressors, measured by combining the Impact of Events Scale and Life Events Scale, identified powerful or severe impacts on well-being for 30% of nurse respondents in this study, theoretically placing them at risk for CF. However, qualitative data did not complement the results of the Life Events Scale, and 55% of the nurses described their overall work experiences as “life-affirming and rewarding.” The participants provided multiple sources of their work-related stress, including subcategories of communication breakdown, work environment/institution, and care-driven factors.
Conclusions: Overall, oncology nurses experienced positive reinforcement at work and they had little concern about individual or organizational effectiveness. Positive experiences offset the negative and balanced out the risk for CF.
Interpretation: The identification of personal and social contributors, as well as solutions to work-related stress, supports the philosophical premises (i.e., conceptual model) that the circumstances that place a nurse at risk for CF are socially constructed. Nurses can achieve greater empathy through self-understanding and translate this learning to patient care.
Jump to a section
Work-related stress (WRS) has many sources and it can cause burnout or place a nurse at risk for compassion fatigue (CF) (Sabo, 2006). As contextual factors change, oncology nurses must continually monitor their workplace experiences for sources that increase their vulnerability to WRS. The purpose of this descriptive, mixed-methods study was to examine factors that influence a nurse’s perceived quality of work life and risk for CF. For this study, CF was broadly defined as fatigue, emotional distress, or apathy resulting from the constant demands of caring for others. The authors explored nurses’ reports of positive and negative experiences for factors that might be modifiable and could be translated into a responsive prevention program to improve the nurse’s satisfaction with his or her work in cancer care and ability to manage WRS. The expectation is that improved nurse satisfaction will improve the delivery of care to patients. The specific aims were to describe the (a) relationship among nurse characteristics and perceived quality of work life, (b) relationship between personal life stress and perceived quality of work life, and (c) the nurse’s beliefs about his or her risk for CF.
Background
Relationships among the nurse, patients, and family members, as well as the nurse being a witness to suffering, are common factors examined in studies of the meaning of oncology nursing (Cohen, Ferrell, Vrabel, Visovsky, & Schaefer, 2010; Figley, 2002; Lewin, 1996). Lewin (1996) described the role of compassion in psychotherapy to include a complex set of feelings, ideas, reactions, and interpersonal dynamics that reflect an appreciation for and understanding of the other’s pain and suffering. Conversely, CF may be understood as a loss of this balance and the substitution of hope with hopelessness and loss of personal well-being (Figley, 2002). The authors believe that fatigue of any kind, including that of compassion, is an important factor in the psychological and possibly physical health of oncology nurses. This phenomenon and the scope of contributory and mitigating factors have been studied in a variety of ways since it was first defined by Joinson (1992). Representative reports are summarized here.
Sources of Work-Related Stress
Barnard, Street, and Love (2006) evaluated 101 oncology nurses for job stressors, perceived support by other nurses, and levels of burnout (a proxy for CF), as well as the relationships among these three variables. Ninety-four percent of the nurses identified two main work stressors: being overwhelmed with the amount of work and poor communication between physicians and nurses. The stressors were ubiquitous. The relationships among stressors and depersonalization, or stressors and emotional exhaustion, showed significant positive correlations.
Meadors and Lamson (2008) studied 185 healthcare providers in a pediatric intensive care unit for work stressors and predicted that personal issues would contribute to work stress. They evaluated stressors related to the personal life of study participants within a previous 12-month period and the feelings that participants had about their personal stressors. Study results demonstrated that individuals with lower personal stress levels showed lower work stress, suggesting that control of personal stress can reduce personal and WRS. In addition, these participants practiced more healthy nutritional and exercise routines and they set boundaries to manage life and work stressors. Individuals with higher personal stress levels also showed higher levels of WRS. Humor and time spent with supervisors did not correlate with decreasing stressors. Similar observations were made by Robins, Meltzer, and Zelikovsky (2009).
Quinal, Harford, and Rutledge (2009) studied the individual risk factors of 43 oncology nurses. Forty-four percent had intrusive thoughts about patients, had disturbing dreams about patients, and woke often. They were irritable, hyper vigilant, easily startled, and had difficulty concentrating and sleeping. These factors indicated secondary traumatic stress (STS).
On the theme of staffing, Wenzel, Shaha, Klimmek, and Krumm (2011) discussed how nurses experienced work on units that were short-staffed. They accurately predicted that staffing issues would increase work stress. Focus group discussions generated solutions (e.g., a supportive work environment would consist of modifying paperwork to allow more nursing time to assist in family grieving). Wenzel et al. (2011) concluded that support should include counseling and mechanisms to allow nurses to verbalize their feelings to coworkers. Focus group members went further to suggest that the work schedule should allow for small break times during the day for revitalization. This study situated the risk for burnout within the structure of the care delivery system. However, Ba, Early, Mahrer, Klaristenfeld, and Gold (2014) evaluated the link between employer-structured support programs and CF and found no clear reduction in risk of WRS; however, the programs did improve professional job satisfaction and, therefore, might have had an indirect effect.
Applicability Across Patient Populations
WRS and the risk for CF are not unique to cancer care and studies of other groups of nurses were instructive as well. Dominguez-Gomez and Rutledge (2009) examined the experiences of 67 emergency department (ED) nurses and showed that 46% of nurses had intrusive thoughts about patients, 43% reported emotional numbing and decreased levels of activity, and 52% reported avoidance of patients. Twenty-seven percent of the nurses became emotionally distressed when they inadvertently thought about various work situations. The authors discussed how emotionally charged memories negatively affected the nurses’ abilities to provide emotional support to patients and their families.
Potter et al. (2010) examined the experiences of 153 participants (i.e., nurses, patient care technicians, and radiation therapy technicians) who were employed in outpatient and inpatient oncology. CF and burnout were assessed using the Professional Quality of Life Scale (ProQOL). The average burnout score was 21.5, and the average CF score was 15.2. Scores greater than 23 for burnout and scores greater than 18 for CF indicate high risk. According to this measure, these nurses were not experiencing CF or burnout. Potter et al. (2010) noted that no relationship existed between education and CF and burnout among nurses, suggesting that educational preparation is not a factor.
Hooper, Craig, Janvrin, Wetsel, and Reimels (2010) also used the ProQOL and compared the interactions among CF, burnout, and compassion satisfaction (CS) in ED nurses (n = 49) and nurses from three specialty services, intensive care (n = 32), oncology (n = 12), and nephrology (n = 16). Regardless of the specialty, the nurses showed moderate to high levels of CF. Twenty-seven percent of oncology nurses scored high for CF (a score greater than 27) compared to total scores of 26.6. For burnout, oncology nurses scored high: 25 compared to 15.6 for the total group. The authors identified a significant inverse relationship between CS and burnout among this cohort of oncology nurses.
The literature has described some of the variables that place the nurse at risk for WRS and CF, revealing the complexity of the phenomenon. However, sample populations and size differed, findings were equivocal, and factors varied across type of facility and patient population. This may be related to the highly personal nature of WRS and the fluctuation of workplace factors. The studies employed surveys and standardized questionnaires, with sample sizes ranging from 9 (Carter, Dyer, & Milken, 2013) to 153 (Potter et al., 2010). Few studies incorporated personal in-depth interviews, which, as a method of data collection, holds high promise to capture the personal dimension and uncover aspects of a phenomenon that is socially constructed. The fact that WRS and CF persists as issues in cancer care demonstrates that a need exists to continue to expand the understanding and pursue prevention strategies using a highly personal approach, engaging the nurse in the process of thinking about his or her risk, and soliciting recommendations. The authors of the current article presumed that engaging in introspection via in-depth interviews would generate complex data that would complement and augment the information collected using surveys, as well as provide solutions and insights from the participants.
Conceptual Model
The nurse’s experience of CF may be considered a consequence of the social environment; therefore, principles from social constructivism were applied to frame the aims of the study, to select mixed methods of data collection and analysis, and to identify ways to mitigate the impact of WRS. Social constructivism is a well-established approach to examining personal/social phenomenon. The term social construct refers to meanings, notions, or connotations that are given to events that occur in a social context (Berger & Luckmann, 1966; Butt, 2001; Neimeyer & Levitt, 2000; Stam, 2001; Thibodeaux, 2014). For the nurse working in cancer care, he or she gives meaning to (i.e., interprets) the day-to-day experiences of caring for patients with cancer and their families. This includes a nurse’s reaction to suffering and death, resistance to care, work-related stressors, and the overlap of personal and professional responsibilities. The implication is that CF experienced by the nurse (or his or her risk for CF) is a consequence of the social interaction within a given environment. This encompasses interpersonal encounters, institutional factors, and the meanings given to these by the individual. A major focus of social constructionism is to uncover the ways in which individuals and groups participate in the construction of their perceived social reality—in this case, the risk for CF.
Methods
This descriptive study used mixed methods of data collection and analysis. The application of principles from social constructivism supported the addition of in-depth interviews to the data collection process. The authors presumed that asking the nurses to engage in introspection via in-depth interviews would generate complex data that would complement and augment information collected using surveys, as well as provide solutions and insights from the participants about the social aspects of their work environment and potential contributions to WRS and CF.
The study took place on the hematology-oncology unit of a large urban teaching hospital in Pennsylvania. The unit is comprised of 47 beds and is staffed by about 50 RNs with various levels of educational backgrounds (e.g., BSN, associate degree, diploma). The unit uses a primary nursing care delivery model. Each nurse typically cares for as many as four patients per shift. The diagnoses included solid and liquid tumors, bone marrow transplantation, leukemia, and lymphoma. Patient acuity ranges from mild to comfort measures and hospice care. The majority of the patients have central lines and the floor is wired for telemetry monitoring. Many of the patients are neutropenic and/or severely immune compromised, which increases the acuity of the patient census. Most of the patients require frequent blood transfusions, multiple IV infusions, and polypharmacy.
Participants
The hospital only employs RNs, and all nurses who were employed on the oncology unit were eligible to participate. The authors targeted night- and day-shift employees and enrolled a sample of 20 nurses. The sample size represented 30% of the overall staff (N = 67). Shifts were 12 hours in duration. This work schedule was changed from 8 hours to provide more time away from the unit (i.e., less work days per week). No exclusion criteria was noted. Self-selection sampling strategy were used, resulting in a sample size of 20.
The authors based the sample size on the likelihood of achieving saturation (Morse, 2000). The selection of a sample size of 20 was determined to be sufficient based on the recommendations of multiple sources. Jette, Grover, and Keck (2003) suggested that expertise in the chosen topic justified a reduced number of participants. Lee, Woo, and Mackenzie (2002) examined sample size across cultures and suggested that studies that apply more than one type of data collection need fewer participants, as do those with interviews with the same participant. Finally, according to Bertaux (1981) and Guest, Bunce, and Johnson (2006), 15 is the smallest acceptable sample.
Data Collection
Data were collected using self-report questionnaires (SRQs) and in-depth interviews. Data were collected during an eight-month period. The authors began with surveying the nurses for their level of personal life stress, quality of work life, and sociodemographic characteristics. SRQs were followed by one in-depth interview, conducted by telephone or in person, at a time that was convenient for the nurse and did not compete for time with work responsibilities. Interviews were audio recorded with the permission of the participant and conducted by three of the coinvestigators, who were doctorally prepared nurses.
Variables
Using SRQs, the authors examined three major variables: nurse characteristics, personal life stress, and quality of work life. In-depth interviews collected narrative data on nurses’ beliefs about their risk for CF and their recommendations for minimizing WRS.
Nurse characteristics: Sociodemographic information collected included age, gender, employment status (full- or part-time), years in nursing, years in oncology, education level, marital status, children, and personal experience with cancer. The information was collected using an SRQ prepared by the research team.
Personal life stress: Personal life stress was defined as the situational factors in the nurse’s life that added to perceived stress. These events might include sale of a house, loss of a family member, personal illness, or any situation or event that required the nurse’s attention and added to his or her perception of personal burden. This construct was created by the investigators and was measured using well-developed, widely used instruments: the Impact of Events Scale (IES) (Horowitz, Wilner, & Alvarez, 1979; Weiss & Marmar, 1997) and the Life Events Scale (LES) (Holmes & Rahe, 1967). These instruments are complementary measures of the individual and cumulative events in the person’s life that contribute to the total experience of stress. According to the authors, as units of life change increase, so does the risk of illness (proxy for stress).
The IES measures the stress of an event that occurred within the past week. Sundin and Horowitz (2002) reported the psychometric properties for the two subscales of intrusion and avoidance. For IES intrusion, the mean alpha was 0.86 (range = 0.72–0.92); for IES avoidance, the mean alpha was 0.82 (range = 0.65–0.9). Using the 0.8 criterion set by Carmines and Zeller (1979), both IES subscales are consistent, indicating that each measures a very similar, if not the same, construct.
The LES measures the composite stress during a 12-month period and was originally designed to measure post-traumatic stress. Gray, Litz, Hsu, and Lombardo (2004) reported on the psychometric properties of the LES checklist. The unique value of the LES is its ability to record multiple types of exposure, such as personal experience and witnessing the experiences of another person. For test-retest reliability, the instrument is stable over seven days (r = 0.82, p < 0.001). Twelve of the 14 items produced a kappa coefficient of 0.4 or higher. Gray et al. (2004) reported that the LES demonstrated strong convergence with measures of psychopathology known to be associated with trauma exposure. Using the IES and LES helped the authors of the current article to differentiate stress that was situational versus related to lifestyle.
Quality of work life: Quality of work life was defined as the nurses’ perception of stressors associated with their role as a nurse in general and their job in particular. According to the literature, work stress is a major risk factor for CF. Quality of work life was measured using the ProQOL. The ProQOL is a 30-item, five-point Likert-type scale ranging from 1 (never) to 5 (very often), measuring the negative and positive aspects of working with people who experience stressful events in the course of their work within the past 30 days (Stamm, 2010). The instrument has subscales for compassion satisfaction, burnout, and STS. According to Stamm (2010), scores lower than 22 show low levels of each, whereas scores of 42 or higher show high levels of burnout and secondary stress. Scores in the 23–41 range are considered average. The ProQOL has three subscales and has been tested extensively and found to be reliable, with reliabilities for CF (0.81), burnout (0.75), and compassion satisfaction (0.88) (Young, Cicchillo, Derr, & Bressler, 2011). The questions on each subscale are summed by the participant for a mean score. This score indicates if the individual is at a low, average, or high level of compassion satisfaction, burnout, and STS.
Nurses’ beliefs and recommendations: Nurses participated in one 30–50 minute audio recorded interview and explored the nurse’s experiences in oncology nursing and how the nurse personally managed WRS. The interview questions were designed to explore factors that would not be captured in the SRQs.
Procedures
The study received approval from the institutional review board of the health delivery system (Tenet Health) and the associated university medical school. One member of the research team was employed on the unit and served as the recruiter. She posted and distributed study information to all staff and provided contact information for the principal investigator. Nurses who expressed interest gave written, informed consent, and were given an envelope containing the SRQs. Each participant anonymously completed the SRQs, sealed them in an envelope, and deposited the envelope in a collection box. The nurse was scheduled for the interview at the time of enrollment. To ensure confidentiality, interviews were conducted by experienced qualitative research faculty, who were not employed on the unit. Interviews were conducted in a private location and at a time convenient for the nurse. The participants were not identified by name on either interview transcripts. Confidentiality of data files was achieved by separating coded information from personal identifiers.
The participants were assured that they could withdraw from the study at any time, for any reason, without question or consequences. All participants were asked a set of questions that provided an in-depth description of their observations, feelings, and recollections of their experience working in cancer care. Interview sessions were conducted either in person or via phone. See Figure 1 for the list of questions and prompts.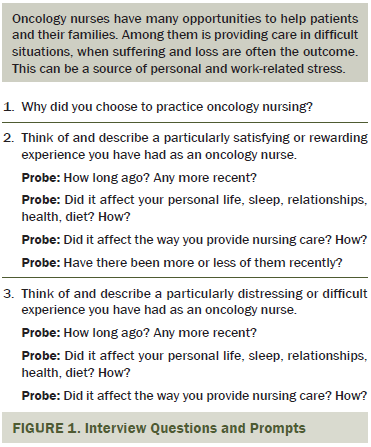
Data Analysis
Survey responses were entered into a database using unique identification numbers. Interviews were transcribed verbatim by a member of the research team who was not a nurse working on the unit. The transcriber was trained by the principal investigator, and the transcription process was continually monitored by the principal investigator to ensure accuracy in capturing all content on the audio recording, as well as inclusion of pauses. During this vetting process, information that linked the interview with the participant’s identity was omitted from the audiotape before transcription.
The authors analyzed responses to the SRQs using descriptive statistics reported as frequencies, percentages, distributions, means, and standard deviations. The authors identified the work-related variables associated with higher stress and separated these into items that are under the nurse’s control and into items that are not (i.e., determined by the employer). Audio recorded interviews were de-identified, transcribed, and imported into NVIVO® 10, a qualitative analysis software program. Qualitative analysis was conducted by the principal investigator and a co-investigator to identify themes and common experiences among participants. The transcripts were coded at three levels: concepts, conceptual categories, and themes that comprised multiple conceptual categories. The authors began analysis using simple thematic content analysis (Clark & Creswell, 2008; Guest, MacQueen, & Namey, 2011) guided by predetermined conceptual categories of (a) a nurse’s perceived quality of work life, (b) personal life stress, (c) a nurse’s belief about his or her risk for CF, and (d) recommendations for minimizing work-related stress. The themes were compared to the summary of responses on the LES, IES, and ProQOL. Guba’s (1981) criteria for assessing the trustworthiness of naturalistic inquiries was applied. In addition, the authors applied Lincoln and Guba’s (1985) criteria for establishing credibility and confirmability. This included rigorous data-cleaning procedures and double checking of transcriptions. During thematic analysis, the investigators used peer debriefings until consensus was reached and new themes were identified in the data. Saturation occurred after about a dozen interviews, but the authors completed all 20 because the nurses had already volunteered to be interviewed.
Results
Sample Characteristics
Twenty female participants took part in the interviews. Sociodemographic information can be found in Table 1.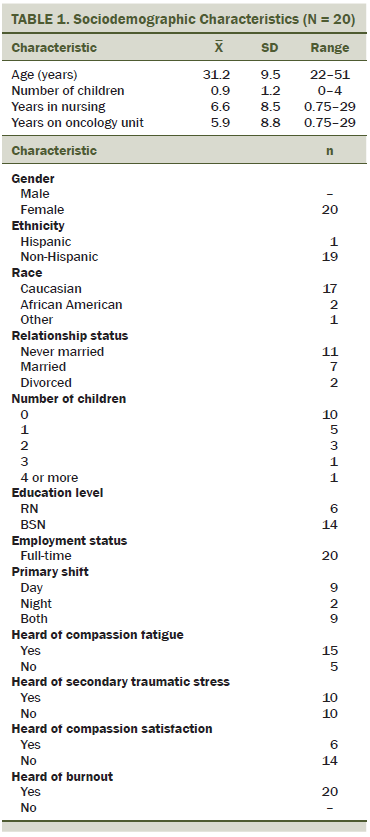
Personal Life Stress
Personal life stress was conceptualized as a combination of the IES and LES. This variable captures how stressors in the nurse’s personal life might contribute to her risk for CF. The questions on each subscale were summed by the participant for a mean score. This score indicated if the individual is at low, average, or high level of compassion satisfaction, burnout, and STS.
Impact of Event Scale: Scores on the IES measured the level of stress a situation might cause, as well as two distinct responses to stress: intrusion (the preoccupation with stressful events in thoughts, dreams, and feelings) and avoidance (evading feelings or reminders of a stressful situation) (Kvaal, Engedal, & Ulstein, 2013). Eleven of the participants had scores in the category of no meaningful impact category, three in mild impact of event, five in powerful impact, and one in severe impact. The majority of participants (n = 14) reported either no or mild impact from stress with their current clinical responsibilities. However, six participants experienced high impact scores, suggesting that caring for patients with cancer may cause a powerful or severe impact on well-being. In looking at intrusion, 19 of the nurses experienced no (n = 13) to mild (n = 6) symptomatology; whereas the remaining individual screened positively for moderate impact. These results are duplicated identically when assessing for avoidance symptomatology. No participant scored in the severe range for intrusion or avoidance (see Table 2).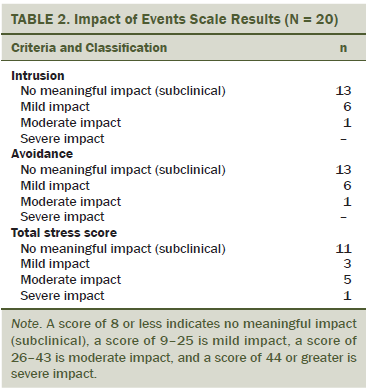
Life Events Scale: Forty-three events were documented, each with a different value, and each participant’s individual score was calculated at the end of the test. The mean score was 120.95 (SD = 86.45). Two events with the highest occurrences were Christmas and vacation, with 10 and 9 participants checking “yes,” respectively. Other test items with high frequencies were a large mortgage or loan, beginning or ending school or college, and a change in sleeping habits, each of which had 7 participants check “yes.” The individual scorings resulted in 14 participants having a low to moderate risk of personal stress affecting their health in the near future, and 6 participants having a moderate to high risk.
Professional Quality of Life Scale: The ProQOL measures both CS and CF. CF is further defined in terms of both burnout and STS. The mean scores were CS, 39.75 (SD = 8.15); burnout, 19.5 (SD = 5.65); and STS, 20 (SD = 4.9). Interpretively, 10 participants scored above average or higher regarding CS. The remaining 10 scored within the average range. In the area of burnout, 14 participants expressed low levels of burnout; the remaining 6 had the expected or average level of burnout. Finally, 14 had low levels of STS; the remaining individuals scored within average limits. None of the participants’ scores demonstrated either low levels of CS or high levels of burnout and STS.
Nurses’ Beliefs About Relationship Between Personal and Work-Related Stress
The qualitative data did not complement the results of the LES, which found six participants to have a moderate to high risk of negative effects. On the contrary, 11 nurses described their overall work experiences as “life-affirming and rewarding.” Only one participant described how negative feelings from work carried over into her personal life and manifested as “insomnia, negative reminders of own loss, sadness, and bad dreams.” Two participants recalled “obsessing” over cases, suggesting they were “too close” at times and resulting in “seeing only the bad.” However, qualitative reports matched the IES finding that 19 of the 20 nurses experienced no to mild symptoms.
Nurses’ Beliefs About Sources of Work-Related Stress
The participants described multiple sources of WRS. These were sorted into subcategories of communication breakdown, work environment/institution, and care-driven factors.
Communication breakdown: A major source of WRS was the perception of deterioration in the quality and quantity of communication between nurses and physicians, nurses and family members, nurses and the patient, and the patient and the family. An example is offered by one of the nurses.
We had one particular patient who I knew wasn’t doing well [but] the interns and residents didn’t want to do anything about it. That’s very frustrating when the interns and residents come and go so quickly, and we know our patients. I think sometimes they don’t trust us or listen to us. But maybe [the patient’s suffering] could have, maybe, been prevented if they had listened to us. That’s what’s been really frustrating as an oncology nurse sometimes with the newer interns and residents in a learning facility.
One nurse commented on the breakdown in communication between her and her patient.
[The patient] didn’t want to take any kind of medicine and she didn’t want to take in any oral; she got very drowsy, anxious, and angry, and she would not let us take care of her because she thought we don’t make choices for her treatment that would make her more comfortable. We did not have a meeting of minds. . . . It was hard for me because all I wanted to do was make her feel as comfortable as possible.
When asked about communication between patients and family members as a source of WRS, one nurse commented,
Yes, yes with us definitely. Because, you know, who wants to tell their family that their loved one wants to give up on the treatment? A patient told one of the nurses that she didn’t want to go through the treatment anymore, so that nurse said “you need to tell your family,” but she never did.
Work environment/institution: The structure of the work environment contributed to WRS. This included nurses’ opinions that their personal needs were ignored, the patient load was too heavy, assignments were uneven, and staffing changes were disruptive. For example, one nurse made the following observation.
I work in a very high-stress acute care setting. But I also think that, on top of that, there is a lot of additional stress from working in a hospital that, at times, doesn’t have the proper resources, or nursing staff turnover is high and new nurses are hired without sufficient experience. Before we eliminated nursing assistants, our ratios could go up to six patients per nurse. It was overwhelming because the nursing assistants knew they weren’t going to be here long so they were not always compliant. I’ve verbalized that to administrations, but there’s really nothing they can do.
Work environment/institution issues compounded stress by frustrating the nurse’s efforts to provide the best possible care. One nurse said, “If I have a really busy assignment, I don’t feel that I can develop as close of a relationship with my patient as I would like. I don’t have the time to talk to them. The tasks take priority.”
Care-driven factors: The third source of WRS and contributor to the risk for CF originated from the actual care provided to the patient. Nurses recalled “demanding family members, discourteous family members, patient’s unreasonable expectations, and frustrated efforts to meet the patients’ needs.” One participant reported being disturbed by occurrences of extraordinary measures that she believed were unethical.
I remember one patient who would constantly call and ask all kind of stuff. She was very demanding and everyone used to try to get away because her care took additional time. . . . She was just very needy. And she wasn’t very sick. She was a grown woman, but scared. . . . She wanted somebody in the room with her. . . . It was a lot to handle.
On occasion, the treatments were more than the nurse could emotionally handle. One nurse commented on extraordinary care as if watching from outside.
You can tell that the patient doesn’t want to go through any more, but due to friendship or promises or something, the doctor is giving false hope to family and to the patient that she will push through. Realistically, she is suffering and it seems unethical to nurses that the care we are giving is making her go through the pain and suffering . . . knowing that she is not going to make it. Over the weekend she coded and she was revived, and now she is brain dead. She could have passed peacefully. That kind of thing bothers me.
Several participants (n = 5) described self-doubt when their idealized image of themselves as “the best nurse that I can be” did not coincide with their evaluation of the care they provided. One nurse commented that she “recognized this as unrealistic” but it was still problematic.
Maybe if I could have spent some time with her the next day. I spent so much time with her over the last week. You know, and it was like what, you know, you get to start thinking, like, not at home, but like when you park your car in the driving lot and drive home and when you drive you reflect on your day and think about what could I have done to make it better . . . you know what I mean. Like try and manage stuff which would have been better, you know?
Recommendations for Minimizing Work-Related Stress
The participants liberally offered suggestions on how to mitigate the effects of WRS and, thereafter, decrease their risk for burnout and CF. The main categories were personal strategies and institutional change. When asked where they saw themselves working in five years, 75% saw themselves working in cancer care. Some participants stated they might go back to school for an advanced degree and return to cancer care in a different role. Most nurses offered examples of ways that they personally managed their risk for CF. Three subcategories of tactics were internal dialogue, defusing stress, and maintaining perspective. Internal dialogue was the self-talk practiced by nurses during stressful events associated with work. Self-talk served to clarify their intentions (i.e., maintain perspective), relieve their tensions (i.e., defuse stress), and remind them of the nursing ideal (i.e., maintain perspective.). Institutional change included suggestions for improving the work environment. Subcategories included nurse-driven changes and policy changes. Figure 2 contains a list of recommendations for preventing CF.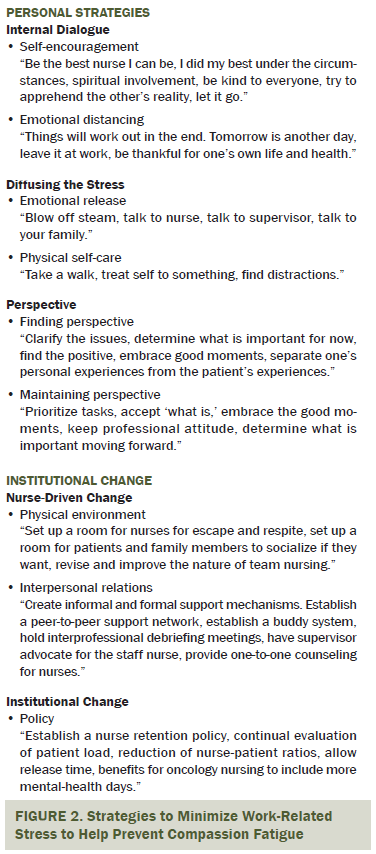
Discussion
A majority of participants (n = 14) reported no or mild stress, and no nurses reported intrusive or avoidance behaviors of a severe magnitude. This differs from findings in Dominguez-Gomez and Rutlege (2009) on WRS in ED nurses and a report from Ba et al. (2014) that reported on oncology nurses (N = 432) experiencing intrusive thoughts (46%), emotional numbing (43%), and avoidance (52%). Thirty percent of the participants in the current article identified powerful or severe impacts on well-being from personal life events.
Oncology nurses in the current study scored average for compassion satisfaction and recorded moderate-to-low scores for burnout and secondary stress (i.e., CF) on the ProQOL. Their average score for CS was slightly less than that which Stamm (2010) considered the best possible combination and score for the ProQOL: high compassion satisfaction and moderate-to-low burnout and STS. These scores reflect a person who experiences positive reinforcement at work. Accordingly, they are good influences on their colleagues and their organization (Stamm, 2010). The findings of the current article differed from the two studies that used the ProQOL on inpatient oncology units with nurses and support staff. Potter et al. (2010) showed average scores for CF and average-to-high burnout scores in oncology nurses and technicians. Hooper et al. (2010) showed moderate-to-high levels of burnout and CF in oncology nurses. Both studies recorded nurses with high burnout scores, whereas no nurse in the current study scored high for burnout. Similar to findings from Hooper et al. (2010), oncology nurses showed a significant inverse relationship between CS and burnout, meaning that nurses in the current study were able to feel satisfied or invigorated by their work.
Unique to the current study was the inclusion of individual interviews to pursue solutions and prevention strategies by focusing on the nurses’ personal and work-related stressors that contribute to risk for CF.
Recommendations to mitigate WRS focused on two areas, institutional change and personal change. Institutional changes involved modifications to the work environment, improved intra- and interprofessional communication, and creating new policies. Suggestions ranged from optimizing the concept of team nursing, to creating a respite room for floor nurses to mentally recharge, to increasing mental health days and release time when feeling overwhelmed. Although many nurses agreed that these changes could lower stress, the literature is not supportive of this idea. No relationship between organizational support and the incidence of burnout was found by Barnard et al. (2006). Ba et al. (2014) concluded that organizational change did not directly protect nurses from CF, but could contribute to CS.
Personal strategies involved initiating self-care activities, diffusing stress through verbalization, and incorporating a new perspective of the situation. Neville and Cole (2013) substantiated the use of self-care behaviors in reducing CF. Wenzel et al. (2011) listed self-care activities as positive activities to support oncology nurses dealing with bereavement and STS exposure from experiencing patient death and dying; therefore, linking positive effects of self-care to STS. However, in searching the literature, the use of internal dialogue, which was commonly echoed as a modifier of stress, has not been fully studied. Research is needed to describe how internal dialogue might build resiliency and reduce risk for CF.
Nurses articulated the challenges and rewards of oncology nursing and described establishing deep relationships with patients and their families. The heavy physical and emotional demands of oncology nursing were felt, including the suddenness with which a patient’s condition might change, leading to distress and a lack of closure. In general, the participants believed that maintaining a healthy work-life balance, leaving the “job” at work, and focusing on self and family outside of work were all essential to risk reduction. When asked, “What would you be doing in five years,” 18 of 20 nurses expressed certainty that they would remain in oncology nursing, suggesting that, for the majority of participants, the rewards of oncology nursing outweighed the challenges.
Limitations
The sample size was relatively homogenous and did not include any male nurses who may have had a different experience with patients, physicians, and family members. They may offer a unique set of personal strategies for minimizing WRS. The nurse manager was a member of the research team, which may have positively or negatively influenced participation in this study. The nurses were employed on a unit with 12-hour work shifts. This arrangement was implemented to reduce the number of work days per year. How this alternative work schedule impacts WRS is unknown. In addition, oncology nurses who work in eight-hour shift schedules may experience WRS differently. Lastly, the sample was homogenous with respect to race and ethnicity. A more sociodemographically diverse sample is needed to fully understand racial and cultural variants and their relationship to CF.
Implications for Nursing Practice
The identification of personal and social contributors, as well as solutions to WRS, supports the philosophical premises (i.e., conceptual model) that the circumstances that place a nurse at risk for CF are socially constructed. In addition, to the nurses’ interpretations of events, the contextual factors include patients, families, institutional policies, and peer interaction. It follows that efforts to reduce risk for and the prevention of CF will need to be situated in social context and involve institutional and interpersonal changes.
Two important outcomes of this study and an aspect of the methodology have clinical implications. No significant relationship was noted between events in the nurse’s personal life and risk for CF. The data clearly place the major source of the risk for CF in the social aspects of the work environment. In addition, nurses identified positive and negative work-related factors that contribute to the risk for CF. Some factors were similar for all nurses; however, others were person-specific. The duality of the oncology nursing experience can become the starting point for developing prevention programs that are both personal and unit-specific.
A program to mitigate the risk for CF can be personal and social. Nurses who are aware of their risk for CF and who wish to gain a better understanding of WRS might self monitor. They may track their reactions to events at work using the IES and track changes in their level of compassion using the PRoQOL. Tracking can be done with paper and pencil instruments or with a smartphone app called Provider Resilience (National Center for Telehealth and Technology, 2015). This mobile app was developed by the creators of the ProQOL and is available at no cost. The application allows daily graphing of responses to ProQOL questions and provides reminders to the nurse to value her life; gives supportive statements, instructive videos, and advice on stress reduction; and illustrates simple physical exercises to promote health. Oncology unit directors may schedule periodic individual meetings to discuss the nurse’s experiences and explore strategies to reduce the nurse’s personal risk. Unit leaders may organize nurse-led meetings to discuss experiences and identify ways to modify the work environment to facilitate stress control and reduction. The recommendations proposed by the nurses who participated in this study may be offered as discussion points to generate practical suggestions and additional ideas.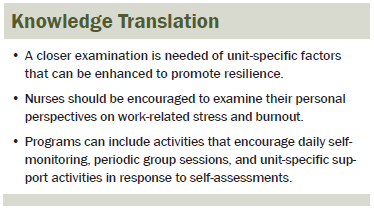
Nurses will be able to achieve greater empathy through self-understanding and translate their learning to engage patients and family caregivers in open conversations to better address their specific needs. These might include sensitive topics such as death and dying, informal caregiver stress, and family CF. The participants’ strategies for minimizing WRS can be translated into a comprehensive prevention program that may be applicable to nurses working in other patient care settings outside of oncology.
References
Ba, A.L., Early, S.F., Mahrer, N.E., Klaristenfeld, J.L., & Gold, J.I. (2014). Group cohesion and organizational commitment: Protective factors for nurse residents’ job satisfaction, compassion fatigue, compassion satisfaction, and burnout. Journal of Professional Nursing, 30, 89–99. doi:10.1016/j.profnurs.2013.04.004
Barnard, D., Street A., & Love, A.W. (2006). Relationships between stressors, work supports, and burnout among cancer nurses. Cancer Nursing, 29, 338–345. doi:10.1097/00002820-200607000-00013
Berger, P.L., & Luckmann, T. (1966). The social construction of reality: A treatise in the sociology of knowledge. Minneapolis, MN: Random House.
Bertaux, D. (1981). From the life-history approach to the transformation of sociological practice. In D. Bertaux (Ed.), Biography and society: The life history approach in the social sciences (pp. 29–45). London, England: Sage.
Butt, T.W. (2001). Social action and personal constructs. Theory and Psychology, 11, 75–95. doi:10.1177/0959354301111007
Carmines, E.G., & Zeller, R.A. (1979). Reliability and validity assessment. Beverly Hills, CA: Sage.
Carter, P.A., Dyer, K.A., & Mikan, S.Q. (2013). Sleep disturbance, chronic stress, and depression in hospice nurses: Testing the feasibility of an intervention [Online exclusive]. Oncology Nursing Forum, 40, E368–E373. doi:10.1188/13.ONF.E368-E373
Clark, V.L., & Creswell, J.W. (2008). The mixed methods reader. Los Angeles, CA: Sage.
Cohen, M.Z., Ferrell, B.R., Vrabel, M., Visovsky, C., & Schaefer, B. (2010). What does it mean to be an oncology nurse? Reexamining the life cycle concepts. Oncology Nursing Forum, 37, 561–570. doi:10.1188/10.ONF.561-570
Dominguez-Gomez, E., & Rutledge, D.N. (2009). Prevalence of secondary traumatic stress among emergency nurses. Journal of Emergency Nursing, 35, 199–204. doi:10.1016/j.jen.2008.05.2003
Figley, C.R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self-care. Psychotherapy in Practice, 58, 1433–1441.
Gray, M.J., Litz, B.T., Hsu, J.L., & Lombardo, T.W. (2004). Psychometric properties of the life events checklist. Assessment, 11, 330–341. doi:10.1177/1073191104269954
Guba, E.G. (1981). Criteria for assessing the trustworthiness of naturalistic inquiries. Education and Communication Technology Journal, 29, 75–91.
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18, 59–82. doi:10.1177/1525822X05279903
Guest, G., MacQueen, K.M., & Namey, E.E. (2011). Applied thematic analysis. Los Angeles, CA: Sage.
Holmes, T.H., & Rahe, R.J. (1967). The Social Readjustment Rating Scale. Journal of Psychosomatic Research, 11, 213–218. doi:10.1016/0022-3999(67)90010-4
Hooper, C., Craig, J., Janvrin, D.T., Wetsel, M.A., & Reimels, E. (2010). Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. Journal of Emergency Nursing, 36, 420–427. doi:10.1016/j.jen.2009.11.027
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218. doi:10.1097/00006842-197905000-00004
Jette, D.J., Grover, L., & Keck, C.P. (2003). A qualitative study of clinical decision making in recommending discharge placement from the acute care setting. Physical Therapy, 83, 224–236.
Joinson, C. (1992). Coping with compassion fatigue. Nursing, 22, 116–121. doi:10.1097/00152193-199204000-00035
Kvaal, K., Engedal, K., & Ulstein, I. (2013). Comparison of anxiety symptoms in spouses of persons suffering from dementia, geriatric in-patients and healthy older persons. Nordic Journal of Nursing Research, 33(4), 4–8. doi:10.1177/01074083130330040
Lee, D.T.F., Woo, J., & Mackenzie, A.E. (2002). The cultural context of adjusting to nursing home life: Chinese elders’ perspectives. Gerontologist, 42, 667–675. doi:10.1093/geront/42.5.667
Lewin, R.A. (1996). Compassion: The core value that animates psychotherapy. Norvale, NJ: Jason Aronson Inc.
Lincoln, Y.S., & Guba, E.G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage.
Meadors, P., & Lamson, A. (2008). Compassion fatigue and secondary traumatization: Provider self-care on intensive care units for children. Journal of Pediatric Health Care, 22, 24–24. doi:10.1016/j.pedhc.2007.01.006
Morse, J.M. (2000). Determining sample size. Qualitative Health Research, 10, 3–5. doi:10.1177/104973200129118183
National Center for Telehealth and Technology. (2015). Provider resilience. Retrieved from http://t2health.dcoe.mil/apps/provider-resilience
Neimeyer, R.A., & Levitt, H. (2000). What’s narrative got to do with it? Construction and coherence in accounts of loss. In J. Harvey (Ed.), Loss and trauma (pp. 401–412). Philadelphia, PA: Brunner Routledge.
Neville, K., & Cole, D. (2013). The relationships among health promotion behaviors, compassion fatigue, burnout, and compassion satisfaction in nurses practicing in a community medical center. Journal of Nursing Administration, 43, 348–354. doi:10.1097/NNA.0b013e3182942c23
Potter, P., Deshields, T., Divanbeigi, J., Berger, J., Cipriano, D., Norris, L., & Olsen, S. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses [Online exclusive]. Clinical Journal of Oncology Nursing, 14, E56–E62. doi:10.1188/10.CJON.E56-E62
Quinal, L., Harford, S., & Rutledge, D.N. (2009). Secondary traumatic stress in oncology staff. Cancer Nursing, 32, E1–E7. doi:10.1097/NCC.0b013e31819ca65a
Robins, P.M., Meltzer, L., & Zelikovsky, N. (2009). The experience of secondary traumatic stress upon care providers working within a children’s hospital. Journal of Pediatric Nursing, 24, 270–279. doi:10.1016/j.pedn.2008.03.007
Sabo, B. (2006). Compassion fatigue and nursing work: Can we accurately capture the consequences of caring work? International Journal of Nursing Practice, 12, 136–142. doi:10.1111/j.1440-172X.2006.00562.x
Stam, H.J. (2001). Introduction: Social constructionism and its critiques. Theory and Psychology, 11, 291–296. doi:10.1177 /0959354301113001
Stamm, B.H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org.
Sundin, E.C., & Horowitz, M.J. (2002). Impact of Event Scale: Psychometric properties. British Journal of Psychiatry, 180, 205–209. doi:10.1192/bjp.180.3.205
Thibodeaux, J. (2014). Three versions of constructionism and their reliance on social conditions in social problems research. Sociology, 48, 829–837. doi:10.1177/0038038513511560
Weiss, D.S., & Marmar, C.R. (1997). The Impact of Event Scale-Revised. In J.P. Wilson & T.M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). New York, NY: Guilford.
Wenzel, J., Shaha, M., Klimmek, R., & Krumm, S. (2011). Working through grief and loss: Oncology nurse’s perspectives on professional bereavement [Online exclusive]. Oncology Nursing Forum, 38, E272–E283. doi:10.1188/11.ONF.E272-E283
Young, J.L., Cicchillo, V.J., Derr, D., & Bressler, S. (2011). Compassion, satisfaction, burnout, and secondary traumatic stress in heart and vascular nurses. Critical Care Nursing Quarterly, 34, 227–234. doi:10.1097/CNQ.0b013e31821c67d5
About the Author(s)
Giarelli is an associate professor in the College of Nursing and Health Professions at Drexel University in Philadelphia, PA; Denigris is a clinical nurse manager at Hahnemann University Hospital in Philadelphia; and Fisher is a professor and Maley is an assistant professor, both in the College of Nursing and Health Professions, and Nolan is a student and research assistant in the Pennoni Honors College, all at Drexel University. No financial relationships to disclose. Giarelli and Denigris contributed to the conceptualization and design. Giarelli, Denigris, Fisher, and Maley completed the data collection. Maley and Nolan provided the statistical support. Giarelli and Fisher contributed to the analysis. Giarelli, Denigris, Fisher, Maley, and Nolan contributed to the manuscript preparation. Giarelli can be reached at eg446@drexel.edu, with copy to editor at ONFEditor@ons.org. Submitted September 2015. Accepted for publication December 12, 2015.

