Perceptions of Stress: Patient and Caregiver Experiences With Stressors During Hospitalization
Background: Hospitalization for a cancer diagnosis and treatment may trigger stressful experiences for patients and family caregivers.
Objectives: The purpose of this study was to identify patients’ and caregivers’ perceptions of stressors during hospitalization and evaluate their education needs.
Methods: A descriptive correlational research design was used to determine whether there is any correlation between the stress perceptions of patients and family caregivers and their need for additional education on health-related issues.
Findings: Patients reported experiencing mild to extreme stress for sleep deprivation, pain, tube and line restrictions, and financial issues. In addition to these stressors, family caregivers also perceived that waiting for test results was a main reason for stress in patients. A positive significant correlation was found between the total sample mean stress scores of patients and their need for additional education on health-related issues.
Jump to a section
Cancer treatment often causes high levels of stress, affecting patients’ quality of life and outcomes and necessitating a holistic approach to care. Patients with cancer may also experience physiologic stress from the disease process or cancer treatment and its side effects. According to Hoffman, McCarthy, Recklitis, and Ng (2009), cancer survivors often report an increased prevalence of serious psychological distress, including patients who have been in remission for five years or longer. In addition, patients with cancer are often hospitalized because of acute conditions. In a study by Numico et al. (2015) on hospital admissions of patients with cancer, 74% of admissions were urgent and 80% were a result of uncontrolled symptoms. The top troublesome symptoms reported by patients in Numico et al.’s (2015) study were dyspnea (16%) and pain (15%). Sixty-one percent of the patients in Numico et al.’s (2015) study were discharged to home, 26% died during hospitalization, and 11% were transferred to a palliative care setting. Being in the hospital may be a stressful experience for many patients because of the unfamiliar environment, feeling a loss of control, noise, an inability to fulfill roles in the family, worries about financial issues, the fear of the unknown, and the unpredictability of their response to cancer treatment (Abuatiq, 2015).
Healthcare providers are in a strategic position to identify and minimize the anticipated stressors of patients and caregivers, particularly during the hospitalization phase. Identifying appropriate interventions to minimize patient and caregiver stressors has the potential to promote effective disease management, encourage family participation in the care plan, and improve the quality of health care. Describing and understanding the stressful experiences of patients and their family caregivers can allow healthcare providers to implement stress reduction strategies that improve patients’ overall satisfaction with the care that they receive during hospitalization. This study describes patients’ self-reports of stress and caregivers’ perceptions of the stress experienced by patients during hospitalization for cancer.
Theoretical Framework
Stress is a highly subjective experience that can prompt an acute onset of physical, emotional, and mental strain, which may affect a patient’s ability to heal and cope (Papathanasiou, Tsaras, Neroliatsiou, & Roupa, 2015). The concept of stress is defined as “a state of mental or emotional strain or tension resulting from adverse or very demanding circumstances” (Lexico, n.d.). Terrill, Gjerde, and Garofalo (2015) defined perceived stress as an individual’s perception of how stressful a particular situation or event is and the extent to which that situation or event is threatening, unpleasant, or out of the individual’s control. For the purposes of this study, the terms stress and stressor were used interchangeably.
The theoretical framework for this study is based on Lazarus and Folkman’s (1987) stress and coping theory, which describes stress and the cognitive appraisal of stressors among individuals. The theory considers the production of stressors by the environment and the response of an individual exposed to these stressors. Cognitive appraisal is a direct result of the individual’s recognition of the stressor; if the stressor is threatening to the physical, psychological, social, and overall healthy well-being of the individual, he or she is more likely to perceive the situation as stressful (Lazarus & Folkman, 1987).
Literature Review
A search was conducted using CINAHL® and PubMed® to establish a scholarly foundation for this study. Search terms included cancer patient, family member, and stress. The search was narrowed to include studies performed from 2009 to 2019.
Some of the studies on stress and patients with cancer that were identified in the literature review focused on post-traumatic stress disorder (PTSD) as a subcategory of stress. In a study by Nipp et al. (2018), hospital readmission rates were 39% among patients with cancer who also were experiencing PTSD compared to those without symptoms of PTSD. Patients in Nipp et al.’s (2018) study who were younger, female, had an increased number of comorbidities, or were diagnosed with genitourinary cancer types reported higher PTSD scores. Symptoms of PTSD experienced by patients were also associated with increased physical symptoms and symptoms of depression and anxiety (Nipp et al., 2018). Similarly, a study by Huang et al. (2018) of older adult patients with cancer experiencing post-traumatic stress symptoms (PTSS) found that 30% had high-acuity cancer, and approximately 7% were categorized as diagnosed with PTSS. PTSS was also associated with higher healthcare costs and increased usage of healthcare services (Huang et al., 2018).
Previous studies on the stressors experienced by patients with cancer have focused on specific cancer diagnoses. Among patients with breast cancer, Pérez et al. (2014) found a significant correlation between PTSS and psychosocial variables, including anxious preoccupation, helplessness, hopelessness, fighting spirit, fatalism, cognitive avoidance, and age. In a study by Draeger, Sievert, and Hakenberg (2018), patients with renal cancer reported that the stressors they experienced included anxiety, pain, nervousness, sadness, worry, and sleeping difficulties. In a study of patients’ family caregivers, Kim, Carver, Shaffer, Gansler, and Cannady (2015) examined possible correlations between the caregiving experience and the development of physical impairments among family members. Kim et al. (2015) found that caregivers of patients with cancer who were under stress were more likely to develop heart disease following their caregiving experience, and caregivers whose spouses were being treated were more likely than non-spousal caregivers to later develop physical issues, such as arthritis or chronic back pain, later in life. Based on their findings, Kim et al. (2015) suggested that implementing stress management interventions as a standard of care for patients with cancer and their caregivers can improve outcomes. In addition to caregivers, healthcare providers play a major role in assessing and managing the stressors of patients with cancer. A study by Kaneko et al. (2013) found that more than 50% of nurses did not feel confident about their ability to assess anxiety and depression in patients with cancer. Oncology nurses in Kaneko et al.’s (2013) study also reported needing additional training and education on how to care for and assess the mental state of patients with cancer.
Based on the literature review, few studies have examined the stress perceptions of patients with specific cancer diagnoses, particularly during hospitalization. In addition, a limited number of studies have evaluated family caregivers’ perspectives of the stressors experienced by patients with cancer during hospitalization or have identified interventions to manage stress in hospitalized patients with cancer. Therefore, the aims of this study were to determine the following:
• What stressors are reported by hospitalized patients receiving cancer treatment?
• What stressors are reported by family caregivers?
• Is there any significant correlation between the stress perceived by patients and caregivers during hospitalization and patients’ self-reported need for additional education on health-related issues?
Methods
A descriptive correlational research design was used. Quantitative and qualitative data were collected from patients with cancer and family caregivers during hospitalization using an updated version of the intensive care unit Environmental Stressors Questionnaire (ESQ).
Sample and Setting
A convenience sampling method was used; data were collected from July 2018 to December 2018. Inclusion criteria were as follows: (a) adults aged 18 years or older; (b) able to read, understand and write in English; (c) oriented to time, person, and place; and (d) either a patient with cancer or a family caregiver of a patient with cancer who was admitted to the hospital for at least 24 hours. The sample consisted of 41 participants, including 26 patients with various cancer types at different stages of disease and 15 family caregivers of patients with cancer who reported being at the patient’s bedside for at least four hours per day during hospitalization.
Institutional review board approval was obtained from a large, nonprofit public hospital located in Sioux Falls, South Dakota. Prior to participation, patients signed consent forms that included a full explanation of the study. To maintain participant anonymity, numeric codes were applied to completed questionnaires and used for data analysis purposes.
Instruments
The ESQ, an updated version of the Intensive Care Unit Environmental Stressor Scale (ICUESS), was used to measure the stress perceptions of patients with cancer during their hospital stay (Cochran & Ganong, 1989; Cornock, 1998). The 50-item ESQ is comprised of quantitative indicators for psychological, physical, environmental, financial, and social stressors. The ICUESS uses a five-point Likert-type scale (1 = not applicable, 2 = not stressful, 3 = mildly stressful, 4 = very stressful, 5 = extremely stressful) (Cochran & Ganong, 1989); however, the rating scale was modified for the ESQ to a five-point Likert-type scale ranging from 0 (not applicable) to 4 (extremely stressful) for data analysis purposes. In this study, the researchers added 10 new variables to the ESQ to examine the effects of technology accessibility on patients’ perceptions of stress during hospitalization. Additional details about the updated ESQ will be published separately. Responses on the 60 items of the updated ESQ are summed, with possible total stress scores ranging from 60 to 300. A mean score of 150 or greater indicates a more stressful experience. The ESQ also includes qualitative indicators that ask participants to self-report their three most stressful items and identify any additional items that they believe should be added to the questionnaire (Cornock, 1998). Rosa, Rodrigues, Gallani, Spana, and Pereira (2010) evaluated the reliability of the ESQ and reported a satisfactory Cronbach alpha of 0.94, with total scores displaying a strong correlation with the generic questions about stress (r = 0.7, p < 0.0001). A data form was also used to capture the demographic information of participants in this study, including gender, ethnicity, and medical insurance status.
Results
The full sample included 26 patients with cancer and 15 caregivers. Patient ages ranged from 24–79 years, with a mean age of 57.35 years. Caregiver ages ranged from 35–76, with a mean age of 66 years. Most patients were male (n = 17), and most caregivers were female (n = 12). In this sample, patient diagnoses included lung (n = 7), breast (n = 6), colorectal (n = 5), pancreatic (n = 4), and prostate (n = 2) cancers, and leukemia (n = 2). Although the hospital length of stay for patients ranged from a minimum of 24 hours to a maximum of 12 days (—X = 5 days), no significant correlation was found between the mean stress scores reported by patients and the length of their hospital stay (r = 0.22, p = 0.15). Demographic information collected from patients and caregivers is presented in Table 1. 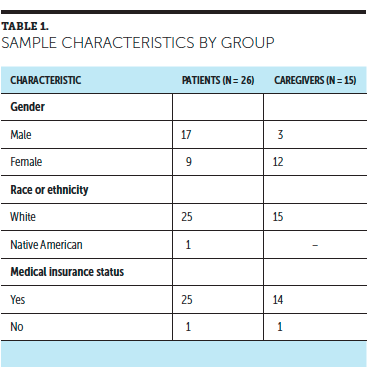
Descriptive frequencies were analyzed to examine the top four stressors reported by hospitalized patients with cancer (N = 26). The top four stressors reported by patients were sleep deprivation, pain, tube and line restrictions, and worries about financial issues. Conversely, the descriptive frequencies that reflected what caregivers (N = 15) perceived to be the main stressors for patients during hospitalization included sleep deprivation, waiting for test results, tube and line restrictions, and worries about financial issues. Patients’ mean stress scores and the perceived stress scores of caregivers are reported in Table 2. 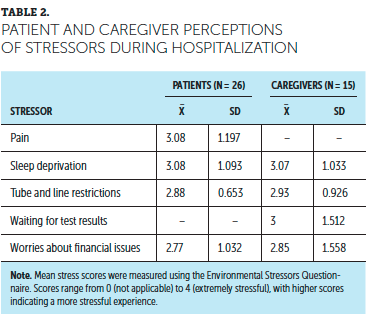
Qualitative themes that highlighted patients’ main stressors during hospitalization included concerns about a lack of health insurance, not qualifying for government-based health insurance, high deductibles, lack of communication from healthcare providers, waiting to receive test results, and experiencing side effects of chemotherapy. The qualitative themes that resulted from caregivers’ reports of perceived stressors for patients included fear of outcomes, lack of control, being away from family members, health insurance costs, fear of cancer not responding to treatment or chemotherapy side effects, not understanding why tests being administered or what they are looking for, and a lack of communication from healthcare providers. Figure 1 illustrates the common qualitative themes of stressors self-reported by patients with cancer and their caregivers. 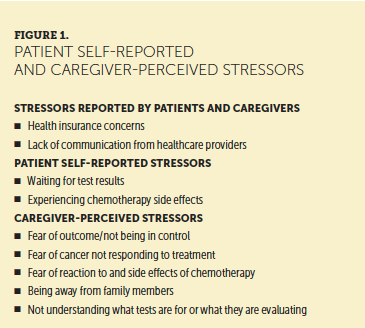
A quantitative analysis was performed using a Pearson correlation coefficient to determine whether there was any correlation between patients’ mean stress scores and item 57 (“Not having any information related to health issues”) on the ESQ. A positive significant correlation was found between the total sample mean stress scores of patients and their need for additional education on health-related issues (r = 0.652, p = 0.01). In addition, a positive significant correlation was found between the total sample mean stress scores of caregivers and their self-reported need for additional education on the patients’ diagnosis and treatment (r = 0.593, p = 0.01). Item 3 on the ESQ (“Please report any educational needs that you may have related to health issues”) was used to collect qualitative responses. Qualitative analysis was performed on this item using ATLAS.ti, version 8. The findings indicated that the primary education needs for hospitalized patients with cancer include a better understanding of the purpose and results of laboratory tests and drug interactions and information on how to manage the side effects of chemotherapy.
Discussion
In this study, pain was one of the primary stressors reported by hospitalized patients with cancer. According to a meta-analysis by van den Beuken-van Everdingen, Hochstenbach, Joosten, Tjan-Heijnen, and Janssen (2016), pain prevalence rates are 39% after curative treatment, 55% during anticancer treatment, and 66% in advanced, metastatic, or terminal disease. Moderate to severe pain was reported by 38% of patients, with the highest prevalence of pain (70%) being reported by patients diagnosed with head and neck cancer (van den Beuken-van Everdingen et al., 2016). Although the World Health Organization offers recommendations for pain management for patients with cancer, cancer pain may still go untreated in many patients (American Association of Critical-Care Nurses, 2016). The results of the current study support the belief that existing pain management protocols may be ineffective. Additional research is needed to ensure that effective pain management strategies are established for patients with specific cancer diagnoses.
In a study evaluating patient-reported distress, Draeger et al. (2018) identified the need for better psychosocial support in patients with renal cancer. The main stressors reported by patients in Draeger et al.’s (2018) study were anxiety (32%), pain (27%), nervousness (26%), and sadness, worry, and sleeping difficulties (20%). Similar to Draeger et al.’s (2018) study, the findings of the current study indicate that patients with varying cancer types often experience sleep deprivation and pain, as well as anxiety about tube and line restrictions and worries about financial issues. Based on these findings, sleep deprivation and pain are common stressors reported by patients with cancer (Draeger et al., 2018). Developing quality improvement measures to decrease the incidence of these stressors during hospitalization is needed.
The results of this study indicate that higher stress perception scores are significantly correlated with the need for more patient and caregiver education on health-related issues, such as information on diagnosis, treatment, and management of side effects. Preventive patient- and family-centered interventions are needed to manage stress among patients with cancer and increase their overall satisfaction with care and treatment. Based on the results of this study, the following stress management strategies are suggested to alleviate stressors and improve patients’ experiences during hospitalization: (a) use targeted pain management protocols for patients with specific types of cancer and (b) enhance the sleep hygiene of patients during hospitalization by providing designated quiet time during night shifts, dimming overhead lighting, and decreasing bedside noise whenever possible. A study by van den Beuken-van Everdingen, de Rijke, Kessels, Schouten, van Kleef, and Patijn (2007) also found that patients feel better supported by their primary care provider and oncology nurses when they have access to all of their laboratory results. Therefore, it is recommended that patients receive thorough education regarding health-related issues (e.g., disease prognosis, potential drug–drug interactions, management of potential side effects from chemotherapy) and the types of laboratory tests that are required and what the results of such tests indicate. Nurses can also support patients by providing them with additional information on how to access their test results, such as education on what to ask about and how to use personal electronic devices or home computers to access results via a secure connection, if available according to the healthcare facility’s information sharing policy. In addition, it is important to ensure open communication with patients and caregivers by providing referral to additional social support, if needed.
Minimizing hospital-related stressors and implementing stress management interventions may potentially decrease stress levels in patients with cancer and their caregivers during hospitalization and increase overall satisfaction with care. To determine effective interventions that address patients’ stress, healthcare providers should perform a complete psychosocial assessment, including careful evaluation of precancer diagnosis trauma and psychiatric history (Cordova, Riba, & Spiegel, 2017). Many studies have evaluated various psychological interventions that can address stress in patients with cancer. In a study by Garssen et al. (2013), a psychological intervention using audio recordings, relaxation exercises, and coping skills was effective in reducing depression and fatigue in patients with cancer. Zhu et al. (2018) also found that providing specific psychological consultation for patients with cancer was effective in reducing patients’ experiences of PTSD. Many studies have reported that yoga can improve the physical and psychological symptoms, quality of life, and immunity markers of patients with cancer (Agarwal & Maroko-Afek, 2018; Diorio et al., 2015; Field, 2016; Ross Zahavich, Robinson, Paskevich, & Culos-Reed, 2013). Urech et al. (2018) found that a web-based stress management intervention (STREss-Aktiv-Mindern [STREAM]) was found to be effective in improving quality of life among newly diagnosed patients with cancer. In addition, in a study on managing pain in patients with breast cancer, mindfulness-based cognitive therapy was found to be effective (Johannsen, O’Connor, O’Toole, Jensen, & Zachariae, 2018).
Limitations
Limitations of this study included the use of a convenience sample, the small sample size, and patient self-report of stressors, all of which limit the generalizability of results. Another limitation is that most of the patients with cancer in this study were receiving treatment in the same oncology unit and, therefore, the experiences that they reported may not be consistent with those of patients with cancer who are hospitalized in other units or receiving treatment in other practice settings.
Implications for Practice
The results of this study can guide healthcare providers in prioritizing the assessment of patients with cancer to ensure that they receive prompt interventions for any stressors that they experience during their hospital stay. In this study, patients reported a lack of communication from healthcare providers as a main stressor during hospitalization, which indicates the need to develop effective communication strategies for patients, caregivers, and healthcare providers. Nurses play a major role in managing patients’ stress, particularly during long-term hospitalization. Therefore, nurses are well positioned to lead an interdisciplinary care team, including physicians, respiratory therapists, rehabilitation therapists, and other members of the healthcare team, with the goal of providing better stress management strategies for patients. To better manage any concerns that patients may have regarding their health insurance coverage, nurses can initiate patient referrals to social workers or case management. To further address patient stressors related to health concerns and anxiety, nurses can provide additional education on cancer treatment, potential side effects, and disease management. Patients in this study also reported experiencing sleep deprivation. Sleep quality can be improved during hospitalization by offering support pillows, dimming lighting, and minimizing interruptions during night shifts. In addition, allowing unrestricted visitation hours to patients with cancer may help family caregivers to participate more effectively in patients’ care during hospitalization and following discharge. According to the American Association of Critical-Care Nurses (2016), allowing unrestricted visitation improved satisfaction among patients and family caregivers and decreased feelings of stress and anxiety. Patients in this study who reported low stress scores also reported greater satisfaction and were able to be discharged in a timely manner with no complications. 
Conclusion
This study explored the primary stressors reported by patients and caregivers during hospitalization and provided recommendations to help decrease stress among patients with cancer. Future research can use this study to improve policies and standards of care aimed at decreasing stressors for patients and caregivers while in the hospital. Providing holistic patient care and pain management interventions targeted to patients’ specific diagnoses, enhancing the quality of sleep during hospitalization, improving patient–provider communication, and including patients and close family members in discussions about care plans are some strategies that can address the main stressors as reported by patients and caregivers in this study. Developing stress management interventions can help to decrease anxiety for patients with cancer during hospitalization and improve overall quality of care. 
About the Author(s)
Alham Abuatiq, PhD, RN, and Robin Brown, PhD, RN, are assistant professors, both in the College of Nursing at South Dakota State University in Brookings; and Brenda Wolles, MS, RN, OCN®, CNL, is a clinical nurse leader at the Sanford University of South Dakota Medical Center and Robin Randall, BSN, RN, OCN®, is the director of medical oncology at Sanford Health, both in Sioux Falls, SD. The authors take full responsibility for this content. Wolles has previously served on advisory boards for Ipsen Biopharmaceuticals. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Abuatiq can be reached at alham.abuatiq@sdstate.edu, with copy to CJONEditor@ons.org. (Submitted June 2019. Accepted September 11, 2019.)
References
Abuatiq, A. (2015). Patients’ and health care providers’ perception of stressors in the intensive care units. Dimensions of Critical Care Nursing, 34, 205–214. https://doi.org/10.1097/DCC.0000000000000121
Agarwal, R.P., & Maroko-Afek, A. (2018). Yoga into cancer care: A review of the evidence-based research. International Journal of Yoga, 11, 3–29. https://doi.org/10.4103/ijoy.IJOY_42_17
American Association of Critical-Care Nurses. (2016). Family presence: Visitation in the adult ICU. Critical Care Nurse, 32, 76–78.
Cochran, J., & Ganong, L.H. (1989). A comparison of nurses’ and patients’ perceptions of intensive care unit stressors. Journal of Advanced Nursing, 14, 1038–1043. https://doi.org/10.1111/j.1365-2648.1989.tb01515.x
Cordova, M.J., Riba, M.B., & Spiegel, D. (2017). Post-traumatic stress disorder and cancer. Lancet Psychiatry, 4, 330–338. https://doi.org/10.1016/S2215-0366(17)30014-7
Cornock, M.A. (1998). Stress and the intensive care patient: Perceptions of patients and nurses. Journal of Advanced Nursing, 27, 518–527. https://doi.org/10.1046/j.1365-2648.1998.00555.x
Diorio, C., Schechter, T., Lee, M., O’Sullivan, C., Hesser, T., Tomlinson, D., . . . Sung, L. (2015). A pilot study to evaluate the feasibility of individualized yoga for inpatient children receiving intensive chemotherapy. BMC Complementary and Alternative Medicine, 15, 2. https://doi.org/10.1186/s12906-015-0529-3
Draeger, D.L., Sievert, K.D., & Hakenberg, O.W. (2018). Analysis of psychosocial stress factors in patients with renal cancer. Therapeutic Advances in Urology, 10, 175–182. https://doi.org/10.1177/1756287218754766
Field, T. (2016). Yoga research review. Complementary Therapies in Clinical Practice, 24, 145–161. https://doi.org/10.1016/j.ctcp.2016.06.005
Garssen, B., Boomsma, M.F., de Jager Meezenbroek, E., Porsild, T., Berkhof, J., Berbee, M., . . . Beelen, R.H. (2013). Stress management training for breast cancer surgery patients. Psycho-Oncology, 22, 572–580. https://doi.org/10.1002/pon.3034
Hoffman, K.E., McCarthy, E.P., Recklitis, C.J., & Ng, A.K. (2009). Psychological distress in long-term survivors of adult-onset cancer: Results from a national survey. Archives of Internal Medicine, 169, 1274–1281. https://doi.org/10.1001/archinternmed.2009.179
Huang, C.H., Kenzik, K., Duhamel, K., Williams, C., Partridge, E., Pisu, M., . . . Kvale, E. (2018). Association between posttraumatic stress symptoms and health care utilization in geriatric patients with cancer: Findings from the patient care connect program. Journal of Pain and Symptom Management, 55, 614–615. https://doi.org/10.1016/j.jpainsymman.2017.12.120
Johannsen, M., O’Connor, M., O’Toole, M.S., Jensen, A.B., & Zachariae, R. (2018). Mindfulness-based cognitive therapy and persistent pain in women treated for primary breast cancer. Clinical Journal of Pain, 34, 59–67. https://doi.org/10.1097/AJP.0000000000000510
Kaneko, M., Ryu, S., Nishida, H., Tamasato, K., Shimodaira, Y., Nishimura, K., & Kume, M. (2013). Nurses’ recognition of the mental state of cancer patients and their own stress management—A study of Japanese cancer care nurses. Psycho-Oncology, 22, 1624–1629. https://doi.org/10.1002/pon.3191
Kim, Y., Carver, C.S., Shaffer, K.M., Gansler, T., & Cannady, R.S. (2015). Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer, 121, 302–310. https://doi.org/10.1002/cncr.29040
Lazarus, R.S., & Folkman, S. (1987). Transactional theory and research on emotions and coping. European Journal of Personality, 1, 141–169. https://doi.org/10.1002/per.2410010304
Lexico. (n.d.). Stress. Retrieved from https://www.lexico.com/en/definition/stress
Nipp, R.D., El-Jawahri, A., D’Arpino, S.M., Chan, A., Fuh, C.X., Johnson, P.C., . . . Greer, J.A. (2018). Symptoms of posttraumatic stress disorder among hospitalized patients with cancer. Cancer, 124, 3445–3453. https://doi.org/10.1002/cncr.31576
Numico, G., Cristofano, A., Mozzicafreddo, A., Cursio, O.E., Franco, P., Courthod, G., . . . Alvaro, M.R. (2015). Hospital admission of cancer patients: Avoidable practice or necessary care? PLOS ONE, 10, e0120827. https://doi.org/10.1371/journal.pone.0120827
Papathanasiou, I.V., Tsaras, K., Neroliatsiou, A., & Roupa, A. (2015). Stress: Concepts, theoretical models and nursing interventions. American Journal of Nursing Science, 4(2), 45–50. https://doi.org/10.11648/j.ajns.s.2015040201.19
Pérez, S., Galdón, M.J, Andreu, Y., Ibáñez, E., Durá, E., Conchado, A., & Cardeña, E. (2014). Posttraumatic stress symptoms in breast cancer patients: Temporal evolution, predictors, and mediation. Journal of Traumatic Stress, 27, 224–231. https://doi.org/10.1002/jts.21901
Rosa, B.A., Rodrigues, R.C., Gallani, M.C., Spana, T.M., & Pereira, C.G. (2010). Stressors at the intensive care unit: The Brazilian version of The Environmental Stressor Questionnaire. Revista da Escola de Enfermagem da USP, 44, 627–635. https://doi.org/10.1590/s0080-62342010000300011
Ross Zahavich, A.N., Robinson, J.A., Paskevich, D., & Culos-Reed, S.N. (2013). Examining a therapeutic yoga program for prostate cancer survivors. Integrative Cancer Therapies, 12, 113–125. https://doi.org/10.1177/1534735412446862
Terrill, A.L., Gjerde, J.M., & Garofalo, J.P. (2015). Background stress inventory: Developing a measure of understudied stress. Stress and Health, 31, 290–298. https://doi.org/10.1002/smi.2554
Urech, C., Grossert, A., Alder, J., Scherer, S., Handschin, B., Kasenda, B., . . . Hess, V. (2018). Web-based stress management for newly diagnosed patients with cancer (STREAM): A randomized, wait-list controlled intervention study. Journal of Clinical Oncology, 36, 780–788. https://doi.org/10.1200/JCO.2017.74.8491
van den Beuken-van Everdingen, M.H., de Rijke, J.M., Kessels, A.G., Schouten, H.C., van Kleef, M., & Patijn, J. (2007). Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Annals of Oncology, 18, 1437–1449. https://doi.org/10.1093/annonc/mdm056
van den Beuken-van Everdingen, M.H., Hochstenbach, L.M., Joosten, E.A., Tjan-Heijnen, V.C., & Janssen, D.J. (2016). Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. Journal of Pain and Symptom Management, 51, 1070–1090. https://doi.org/10.1016/j.jpainsymman.2015.12.340
Zhu, L., Ranchor, A.V., Helgeson, V.S., van der Lee, M., Garssen, B., Stewart, R.E., . . . Schroevers, M.J. (2018). Benefit finding trajectories in cancer patients receiving psychological care: Predictors and relations to depressive and anxiety symptoms. British Journal of Health Psychology, 23, 238–252. https://doi.org/10.1111/bjhp.12283