Pediatric Survivorship: Considerations Following CAR T-Cell Therapy
Background: This article presents an overview of pediatric relapsed and refractory acute lymphoblastic leukemia (ALL) and chimeric antigen receptor (CAR) T-cell therapy in pediatric patients.
Objectives: Acute and chronic post–CAR T-cell effects and considerations are discussed, along with survivorship considerations.
Methods: A case study illustrates the identification and management of physiologic and psychosocial sequelae.
Findings: B-cell aplasia, hypogammaglobulinemia, infections, and cumulative effects of CAR T-cell therapy and other treatments are a concern in the pediatric population. Unique to pediatric and young adult survivors of childbearing potential are implications for post-treatment fertility. Financial toxicities and psychosocial needs require a family-centered approach to interventions that address the impact of CAR T-cell therapy not only on the patient, but also on caregivers and siblings.
Jump to a section
Pediatric acute lymphoblastic leukemia (ALL) is the most common cause of cancer in children (Foster & Maude, 2018). Pediatric ALL accounts for 25% of cancer diagnoses in children younger than age 15 years and 19% of cancers in those aged 15–19 years (Hucks & Rheingold, 2019). Effective treatment strategies related to continuing scientific and clinical research have contributed to cure rates greater than 80% in patients with pediatric ALL (Annesley, Summers, Ceppi, & Gardner, 2018). Unfortunately, relapsed ALL is a significant contributor to childhood cancer mortality. Treatment failure is often seen in patients who have refractory disease to chemotherapy or who have one or more relapses (Forsberg, Das, Saha, & Capitini, 2018). Chemotherapy resistance in refractory and relapsed B-cell ALL demonstrates the need for newer novel therapies, including chimeric antigen receptor (CAR) T-cell therapy.
CAR T-cell therapy is a form of targeted immunotherapy using autologous T cells that are genetically engineered to recognize and attack a specific antigen on malignant cells (Callahan, Baniewicz, & Ely, 2017). The goals for this therapy are for proliferation of the CAR T cells once infused and for persistence for long-term disease surveillance (Grupp, 2014). An article in this supplement by Lamprecht and Dansereau (2019) provides a more in-depth review of CAR T-cell therapy.
Multiple physical and psychosocial issues can complicate the care of patients and their families (Callahan et al., 2017), including relapses, numerous rounds of treatment, and persistent distress over failed treatment. In addition, many patients travel great distances for this specialized treatment because treatment is only authorized at a limited amount of centers. This situation almost always requires temporary relocation for the patient and caregiver.
Because CAR T-cell products are only recently approved by the U.S. Food and Drug Administration (FDA), and longitudinal data continue to emerge from clinical trials, limited data exist about survivorship care for this unique patient population. This article presents an overview of survivorship considerations for pediatric patients with relapsed and refractory B-cell ALL, including the possible late effects from primary treatment before receiving CAR T-cell therapy and long-term issues related to CAR T-cell therapy.
Children and adolescents who have refractory or relapsed ALL and have been extensively treated prior to their CAR T-cell therapy are at significant risk for late effects, particularly those related to the endocrine, cardiac, and neurocognitive systems. Patients are also at risk for secondary malignant neoplasms. The following case study illustrates the treatment exposures typical of a child prior to receiving CAR T-cell therapy.
Case Study
E.J. is a 16-year-old woman with multiple relapses of B-cell ALL, currently in her third remission. E.J. lives with her parents and two siblings in a rural town five hours from the authorized CAR T-cell treating center and two hours from her primary treating center. E.J.’s mother took unpaid leaves from work during treatment. E.J.’s father continued to work, providing medical insurance for treatment.
E.J. was initially diagnosed with B-cell ALL at age 6 years. She received multi-agent chemotherapy according to Children’s Oncology Group (COG) protocol that included vincristine, dexamethasone, daunorubicin, doxorubin, PEG-asparaginase, mercaptopurine, methotrexate, cytarabine, cyclophosphamide, and thioguanine. She completed treatment with minimal complications. Eighteen months after completion of therapy, E.J. relapsed in her bone marrow. She received chemotherapy per COG protocol AALL0433 that included vincristine, doxorubicin, prednisone, asparaginase, cytarabine, etoposide, cyclophosphamide, and methotrexate. She then received a matched unrelated cord blood transplantation using fludarabine, cyclophosphamide, and total body irradiation (TBI) as her conditioning regimen. Transplantation complications included human herpesvirus-6 viremia, Epstein-Barr virus reactivation, acute graft-versus-host disease (GVHD) of the skin and gut, septic shock requiring extracorporeal membrane oxygenation, and acute renal failure requiring temporary continuous veno-venous hemofiltration. Post-transplantation, she developed mixed restrictive and obstructive lung disease and premature ovarian failure.
Three and a half years post-transplantation, E.J. relapsed again in her bone marrow. She was referred for CD19-directed CAR T-cell therapy. T cells were collected, and she received low-dose chemotherapy. She received her CAR T-cell infusion six months after her second relapse. Pre–CAR T-cell therapy lymphodepleting chemotherapy consisted of cyclophosphamide and fludarabine.
Complications from CAR T-cell therapy included cytokine release syndrome (CRS), hypotension requiring vasopressor support, cardiomyopathy requiring long-term medications, respiratory distress requiring continuous positive airway pressure, seizure activity requiring antiseizure medications following CAR T-cell therapy, encephalopathy, and hypogammaglobulinemia from B-cell aplasia.
Acute and Chronic Adverse Effects
As with all cancer therapies, there are immediate risks and side effects with CAR T-cell therapy, as well as actual and potential long-term effects. A primary (acute) side effect after CAR T-cell therapy is CRS. CRS is a systemic inflammatory response resulting from T-cell proliferation. Symptoms can range from mild to severe and may include fevers, headaches, myalgia, fatigue, and anorexia (Smith & Venella, 2017). More severe symptoms may include hypotension, capillary leak, coagulopathy, renal insufficiency, and tumor lysis (Smith & Venella, 2017).
Some patients have experienced neurologic toxicities, such as encephalopathy, aphasia, and seizures. All of these side effects are reversible. E.J. experienced seizures in the immediate period after receiving CAR T-cell therapy and remained on antiseizure medication for the year after CAR T-cell infusion. Consultation and follow-up with neurology specialists can support effective care and, in E.J.’s case, resulted in weaning her from antiseizure medication.
GVHD is a risk for patients who have had an allogeneic stem cell transplantation. The T cells that are collected from these patients are usually donor-derived (Smith & Venella, 2017). Although there is a risk of GVHD, CAR T cells collected after allogeneic stem cell transplantation have not shown a tendency to cause GVHD (Bonifant, Jackson, Brentjens, & Curran, 2016). Patients who have received an allogeneic stem cell transplantation are monitored for long-term signs of GVHD as long as the CAR T cells persist.
B-cell aplasia with resulting hypogammaglobulinemia is a long-term effect of CAR T-cell therapy. CD19-directed CAR T-cell therapy targets any cells that express the CD19 antigen, including normal and malignant B cells. The destruction of normal B cells results in chronic B-cell aplasia, which leads to hypogammaglobulinemia. The targeting of normal B cells is an on-target (targeting the CD19 antigen), off-tumor, and expected long-term toxicity of CAR T-cell therapy (Maude, Teachey, Porter, & Grupp, 2015). B-cell aplasia is used as a marker of CAR T-cell persistence. As long as the CAR T cells persist in the patient, B-cell aplasia persists as well. Hypogammaglobulinemia can increase the risk of infection (Maus, Grupp, Porter, & June, 2014).
Chronic, long-term hypogammaglobulinemia is manageable with scheduled immunoglobulin infusions, either via IV or subcutaneous route. Immunoglobulin G (IgG) levels are monitored monthly. The need for immunoglobulin replacement continues as long as CAR T cells persist. The goal of immunoglobulin replacement is to reduce the frequency and severity of infections. In an analysis of patients with primary immunodeficiency disease, in which pneumonia is the most frequent infection, evidence demonstrated that pneumonia risk can be reduced with higher IgG trough levels up to 1,000 mg/dl (Orange, Grossman, Navickis, & Wilkes, 2010). B-cell immunodeficiencies can lead to chronic otitis media, sinusitis, pneumonia, and bronchiectasis (Mazza & Lin, 2016). After CAR T-cell therapy, pediatric patients with chronic hypogammaglobulinemia are managed with scheduled immunoglobulin replacement and consistent monitoring of IgG level and infection risk.
Some risks are theoretical and have not yet been reported, including malignant transformation, induction of T-cell lymphoproliferative disorders, and production of a replication competent retrovirus (Barrett, Singh, Porter, Grupp, & June, 2014). The effect of CAR T cells and the resulting B-cell aplasia leading to hypogammaglobulinemia on a developing fetus is unknown. With patients and families as part of a treatment plan, providers should discuss pregnancy and effective contraception, particularly when patients are adolescents and young adults.
Because of this new therapy, patients are followed long-term for actual, potential, and theoretical risks. Patients like E.J. who develop severe CRS after CAR T-cell infusion may require long-term cardiac follow-up to monitor or manage cardiac issues, such as cardiomyopathy. For patients who developed seizures during CRS and continue on antiseizure medications, neurologists may need to manage treatment and wean medication. For pediatric patients with long-term hypogammaglobulinemia, clinical immunologists can manage subcutaneous immunoglobulin replacement at home.
The first generation of patients who have undergone CAR T-cell therapy have had refractory or recurrent B-cell ALL prior to receiving the therapy. The majority of these patients have been heavily treated with chemotherapy and radiation prior to undergoing CAR T-cell therapy. Therefore, by the time they are treated, pediatric patients may experience persistent late effects from their primary treatment protocol. These late effects may appear months to years after treatment. As a result, all those involved in the care of the patient, including the primary immunotherapy team and referring providers, must manage the patient at risk for or experiencing late effects.
Survivorship
In cancer care, survivorship focuses on the health of a person after therapy and throughout his or her lifespan. This includes physical, emotional, and financial aspects of cancer that affect the individual and his or her support system (National Cancer Institute, 2019).
Endocrine
Trending growth and development are the most basic indicators of a healthy child. After cancer therapy, other than focusing on surveillance to detect relapse, parents begin to focus on their child’s general health and well-being, including linear growth, weight gain, and cognitive abilities (Hobbie et al, 2010). The endocrine system is often affected by cancer treatment. The hypothalamus and pituitary gland work synergistically to maintain homeostasis. Releasing and inhibiting hormones that regulate end organ function are produced in the hypothalamus and act on the pituitary gland, including the thyroid, gonads, and adrenal glands. The endocrine system can be affected by radiation to the hypothalamic-pituitary axis or to end organs.
Many patients receiving CAR T-cell therapy have previously received relapse therapy that included TBI and allogeneic stem cell transplantation. These patients are at risk for central and peripheral endocrine dysfunction (Dvorak et al., 2011). Growth hormone is often the first hormone affected by cranial irradiation. Dysfunction has been noted with doses of cranial radiation of 1,800 cGy or greater and TBI (Giorgiani et al., 1995; Wohlschlaeger, Mostoufi-Moab, & Bunin, 2015). TBI influences bone growth, exposing epiphyses and the spine to radiation, affecting adult height. TBI can also have an effect on the thyroid gland.
Younger age and the length of time from transplantation have been associated with thyroid dysfunction (Lawitschka & Peters, 2018). Frequent monitoring for elevations in thyroid-stimulating hormone are recommended. Early detection of compensated hypothyroidism and intervention prior to the onset of symptom are essential to maximize growth and development in children. Monitoring for thyroid nodules is also important after TBI (Shimazaki, Kazukawa, Ishida, & Minagawa, 2018). Annual examination of the thyroid is recommended. The use of ultrasound to assess abnormalities is standard of care (Chemaitilly & Hudson, 2014).
Gonadal Functioning and Fertility
Gonadal functioning is often significantly affected following allogeneic stem cell transplantation. Sex, total doses of alkylating agents, and radiation are all important factors (Levine et al., 2018; Wohlschlaeger et al., 2015). Most women and men will be infertile after TBI (Levine et al., 2018; Wohlschlaeger et al., 2015). Although the ovary is fairly resistant to chemotherapy and radiation, the majority of young women will be infertile and need hormone replacement to go through puberty following TBI (Ogilvy-Stuart et al., 1992). The testes are affected differently by treatment. Germinal epithelium exposure to low-dose testicular radiation can cause azoospermia, whereas the leydig cell can continue to produce testosterone after higher doses of radiation (Ash, 1980; Castillo, Craft, Kernahan, Evans, & Aynsley-Green, 1990). Alkylating agents affect gonadal function as well. In the non-transplantation setting, the prepubertal ovary can tolerate total lifetime doses above 25 g and still progress through puberty, but premature ovarian failure is a risk (Friedman, 2015; Kreuser, Xiros, Hetzel, & Heimpel, 1987). Men exposed to cyclophosphamide have been reported to have germinal cell dysfunction at total doses of 7.5–9 g (Aubier et al., 1989; Kenney, Laufer, Grant, Grier, & Diller, 2001). However, the majority of men will retain leydig cell function because these cells are much less vulnerable and are able to function after high doses of alkylating agents (Ginsberg, 2015).
In the case of E.J., she will likely be infertile and will require careful monitoring of ovarian function. Estrogen replacement increases linear growth, but then the epiphyses will close after a period of two years. Therefore, balancing estrogen replacement with growth hormone replacement can maximize linear growth.
Adrenal insufficiency in patients undergoing CAR T-cell therapy would more likely be associated with a history of prolonged corticosteroid therapy, exposure to cranial radiation, or TBI (Wei & Crowne, 2018). These survivors are monitored annually for adrenal insufficiency with morning cortisol levels (Children’s Oncology Group, 2018). In addition, TBI may affect the adrenal gland itself, but this is more common following higher doses of abdominal radiation.
Cardiac
Cardiac late effects of childhood cancer therapy have been associated with several factors: cumulative anthracycline dose, younger age at treatment, female gender, and exposure to radiation (van der Pal et al., 2012). Children who receive both TBI and anthracycline therapy have the highest risks of cardiac late effects. Progressive ventricular dysfunction, congestive heart failure, arrhythmia, and dyslipidemia are known late effects of therapy (Franco & Lipshultz, 2015; Friedman et al., 2017; van der Pal et al., 2012). The Children’s Oncology Group’s (2018) long-term follow-up guidelines provide screening recommendations based on prior treatment. Counseling patients to avoid smoking and participate in aerobic exercise with light weights while maintaining ideal body weight may attenuate other cardiac confounders and decrease cardiac events.
Neurocognitive
Neurocognitive late effects from childhood cancer therapy are well documented and one of the most-studied effects starting with the earliest survivors in the early 1980s (Kadan-Lottick & Kunin-Baston, 2015; Krull et al., 2013; Meadows et al., 1981; Mulhern & Butler, 2004). The combination of intrathecal medication, high-dose antimetabolite therapy, and TBI places children at significant risk for learning disabilities (Cheung et al., 2016). Younger age at time of treatment, female sex, and genetic factors all play a part in the expression of these effects. Common problems other than decreased IQ include slowed processing speed, poor short-term memory, concentration difficulties, and problems with executive function and organization (Cheung & Krull, 2015). Methotrexate leukoencephalopathy can be asymptomatic or acutely cause seizures or stroke, which can also have long-term neurocognitive sequelae (Kadan-Lottick & Kunin-Baston, 2015). The Children’s Oncology Group (2018) recommends neurocognitive evaluations every two years to maximize supportive services for patients in school. Individualized education plans, untimed testing, and resource room accommodations can provide opportunities for improvement in a childhood survivor’s school performance. Early identification and interventions maximize the survivor’s success.
Second Malignant Neoplasms
Prior to receiving CAR T-cell therapy, a pediatric cancer survivor is at risk for second malignant neoplasms (Friedman et al., 2010; Wingard et al., 2011). Etoposide, TBI, high-dose cyclophosphamide, and cranial irradiation are the most significant treatment-related factors. Cancer of the liver, oral cavity, thyroid, and cervix are the most common second malignant neoplasms following TBI and allogeneic stem cell transplantation (Wohlschlaeger et al., 2015). Skin and oral cancer risk increases with chronic GVHD (Chow et al., 2016). Breast cancer risk is associated with radiation to breast tissue. Early mammography and breast magnetic resonance imaging are recommended in this population (Chow et al., 2016). Genetic predisposition will also affect lifetime risk of malignancy, as will lifestyle choices such as smoking. After CAR T-cell therapy, there is a theoretical risk of malignant transformation of the CAR T cells (Barrett et al., 2014). COG guidelines provide detailed guidance in the care of the childhood cancer survivor.
Psychosocial Implications
Many patients undergoing CAR T-cell therapy and their families have been dealing with cancer and its treatment for many years. Parents have lived with the uncertainty of their child’s survival and distress through multiple treatment failures. Post-traumatic stress disorder has been examined in patients, survivors, and their families (Alderfer, Navsaria, & Kazak, 2009; Kazak et al., 1997; Stuber et al., 1997, 2010). In addition to medical concerns, families are also at risk for financial distress and psychosocial issues. The family of a patient undergoing CAR T-cell therapy may need to relocate to another city for at least a six-week period for treatment and return to the medical center every three months for follow-up. In many cases, one caregiver travels with the patient to the treatment center while the other caregiver and any siblings must remain at home, so they can continue work or school. The family must maintain their home and cover typical expenses, as well as the expenses of their temporary home. As a result of the relocation, they may be separated from their social support network. Pediatric cancer has been shown to have an effect on families, including married parents and siblings (Burns et al., 2017; D’Urso, Mastroyannopoulou, & Kirby, 2017; Sulkers et al., 2015; Van Schoors, Caes, Alderfer, Goubert, & Verhofstadt, 2017; Wijnberg-Williams, Van de Wiel, Kamps, & Hoekstra-Weebers, 2015; Yang, Mu, Sheng, Chen, & Hung, 2016). Fitting in within a potentially new hospital environment with new care providers can increase uncertainty and anxiety for pediatric patients and their families.
E.J.’s family came to an urban medical facility from a rural setting. Loughery and Woodgate (2015) report that families from rural areas tend to have a higher financial burden related to less access to medical care and insurance. These families also travel farther distances to pediatric cancer centers.
During the first year following diagnosis, pediatric oncology families are increasingly vulnerable to financial stress (Warner, Kirchhoff, Nam, & Fluchel, 2015). This is related to unplanned hospitalizations and therapies, out-of-pocket expenses, and lack of outside monetary assistance. Financial stress is further compounded by changes in parental employment often related to one parent either decreasing or discontinuing work hours (Miedema, Easley, Fortin, Hamilton, & Mathews, 2008; Warner et al., 2015; Yabroff, Lund, Kepka, & Mariotto, 2011).
There are certain risk factors that increase the likelihood of depression in survivors, including sex, age at diagnosis (specifically adolescence), unemployment, low-income levels, and those with late effects (Bitsko et al., 2016). In several research studies, post-traumatic stress is more prevalent among pediatric cancer survivors with risk factors for depression compared to siblings and other controls (Bitsko et al., 2016; Cupit-Link, Syrjala, & Hashmi, 2018).
Studies report that parents tend to rate emotional distress in patients with cancer higher than the patient’s rating (Rodriguez et al., 2012; Rosenberg et al., 2013; Zhukovsky et al., 2015). Parents who perceived that their child was in greater distress emotionally had higher risks for severe psychological distress themselves, except if the perceived distress was primarily pain (Rosenberg et al., 2013). Uncertainty and fear of relapse is always an underlying concern for families with relapsed and refractory patients. Anxiety is also heightened with novel and experimental therapies because the long-term results and side effects are unknown. When these therapies are only offered at outside institutions, changes in routines and medical practices can compound this anxiety.
Siblings have their own unique set of psychosocial challenges related to disruptions of their normal routines, family separation, and decreased parental attention. These include increased behavioral issues because of sadness, guilt, anxiety, isolation/abandonment, and jealousy. These issues tend to be lessened when addressed with age-appropriate communication within the family (Cincotta, 2015; Cupit-Link et al., 2018).
Because psychosocial effects and financial stressors can severely influence the patient and family, providers—including physicians, nurses, and social workers—can screen and refer families to psychologists, social workers, child life therapists, and creative arts therapists (Bitsko et al., 2016; Pelletier & Bona, 2015). 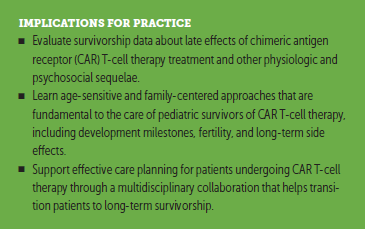
Conclusion
E.J. is three years post–CAR T-cell therapy and continues in remission. CAR T cells still persist, as evidenced by B-cell aplasia. Her survivorship team follows her at home. The immunotherapy treating team also follows her every six months, and follow-up care will continue with the immunotherapy team for 15 years.
Patients undergoing CAR T-cell therapy have received many years of treatment, which may include chemotherapy, radiation, immunotherapy, and allogeneic stem cell transplantation. These factors bring a complexity into the care of these patients that continues into survivorship. As CAR T-cell therapy becomes more successful in prolonging lives, survivorship care plans should include evaluation and intervention for late effects from primary and CAR T-cell therapies. Many of these children and adolescents have been exposed to numerous therapeutic entities and are at substantial risk for significant late effects. A multidisciplinary approach is imperative in caring for these patients. Successful collaboration among immunotherapy teams, referring teams, and survivorship teams are needed to best meet the needs of these patients and their families. The patients require this multidisciplinary approach as they complete CAR T-cell therapy and begin to return to their lives outside of the treatment setting so that early identification and intervention of late effects will attenuate the full impact of these issues. These patients experience many physical and psychosocial stressors. These survivors have a complicated treatment history that may affect their physical and emotional well-being and require physical and psychosocial care and support. Oncology nurses play an integral role in care coordination, education, and anticipatory guidance regarding potential late effects of patients’ primary therapy and CAR T-cell therapy.
About the Author(s)
Colleen Callahan, MSN, CRNP, and Amy Barry, MSN, CRNP, are nurse practitioners in the Division of Oncology, Cancer Immunotherapy Program, Stephanie Fooks-Parker, MSW, LSW, OSW-C, is a social worker, and Laura Smith, MSN, CRNP, is a nurse practitioner, both in the Division of Oncology, Cellular Therapy and Transplant Section, Diane Baniewicz, MSN, CRNP, is a nurse practitioner in the Division of Oncology, Cancer Immunotherapy Program, and Wendy Hobbie, MSN, CRNP, FAAN, is the associate director of the cancer survivorship program, all at the Children’s Hospital of Philadelphia in Pennsylvania. The authors take full responsibility for this content. This supplement was supported by an independent educational grant from Bristol-Myers Squibb. Callahan consults for Novartis Pharmaceuticals. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Callahan can be reached at callahan@email.chop.edu, with copy to CJONEditor@ons.org. (Submitted January 2019. Accepted January 31, 2019.)
References
Alderfer, M.A., Navsaria, N., & Kazak, A.E. (2009). Family functioning and posttraumatic stress disorder in adolescent survivors of childhood cancer. Journal of Family Psychology, 23, 717–725.
Annesley, C.E., Summers, C., Ceppi, F., & Gardner, R.A. (2018). The evolution and future of CAR T cells for B-cell acute lymphoblastic leukemia. Clinical Pharmacology and Therapeutics, 103, 591–598. https://doi.org/10.1002/cpt.950
Ash, P. (1980). The influence of radiation on fertility in man. British Journal of Radiology, 53, 271–278. https://doi.org/10.1259/0007-1285-53-628-271
Aubier, F., Flamant, F., Brauner, R., Caillaud, J.M., Chaussain, J.M., & Lemerle, J. (1989). Male gonadal function after chemotherapy for solid tumors of childhood. Journal of Clinical Oncology, 7, 304–309. https://doi.org/10.1200/JCO.1989.7.3.304
Barrett, D.M., Singh, N., Porter, D.L., Grupp, S.A., & June, C.H. (2014). Chimeric antigen receptor therapy for cancer. Annual Review of Medicine, 65, 333–347.
Bitsko, M.J., Cohen, D., Dillon, R., Harvey, J., Krull, K., & Klosky, J.L. (2016). Psychosocial late effects in pediatric cancer survivors: A report from the Children’s Oncology Group. Pediatric Blood and Cancer, 63, 337–343. https://doi.org/10.1002/pbc.25773
Bonifant, C.L., Jackson, H.J., Brentjens, R.J., & Curran, K.J. (2016). Toxicity and management in CAR T-cell therapy. Molecular Therapy—Oncolytics, 3, 16011.
Burns, W., Péloquin, K., Sultan, S., Moghrabi, A., Marcoux, S., Krajinovic, M., . . . Robaey, P. (2017). A 2-year dyadic longitudinal study of mothers’ and fathers’ marital adjustment when caring for a child with cancer. Psycho-Oncology, 26, 1660–1666.
Callahan, C., Baniewicz, D., & Ely, B. (2017). CAR T-cell therapy: Pediatric patients with relapsed and refractory acute lymphoblastic leukemia. Clinical Journal of Oncology Nursing, 21(Suppl., 2), 22–28. https://doi.org/10.1188/17.CJON.S2.22-28
Castillo, L.A., Craft, A.W., Kernahan, J., Evans, R.G., & Aynsley-Green, A. (1990). Gonadal function after 12-Gy testicular irradiation in childhood acute lymphoblastic leukemia. Medical and Pediatric Oncology, 18, 185–189.
Chemaitilly, W., & Hudson, M.M. (2014). Update on endocrine and metabolic therapy-related late effects observed in survivors of childhood neoplasia. Current Opinion in Endocrinology, Diabetes, and Obesity, 21, 71–76.
Cheung, Y.T., & Krull, K.R. (2015). Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: A systematic review. Neuroscience and Biobehavioral Reviews, 53, 108–120.
Cheung, Y.T., Sabin, N.D., Reddick, W.E., Bhojwani, D., Liu, W., Brinkman, T.M. . . . Krull, K.R. (2016). Leukoencephalopathy and long-term neurobehavioural, neurocognitive, and brain imaging outcomes in survivors of childhood acute lymphoblastic leukaemia treated with chemotherapy: A longitudinal analysis. Lancet Haematology, 3(10), e456–e466.
Children’s Oncology Group. (2018). Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers [v.5.0]. Retrieved from http://www.survivorshipguidelines.org/pdf/2018/COG_LTFU_Guidelines_v5.p…
Chow, E.J., Anderson, L., Baker, K.S., Bhatia, S., Guilcher, G.M., Huang, J.T. . . . Castellino, S.M. (2016). Late effects surveillance recommendations among survivors of childhood hematopoietic cell transplantation: A Children’s Oncology Group report. Biology of Blood and Marrow Transplantation, 22, 782–795.
Cincotta, N. (2015). Helping siblings of pediatric cancer patients. In G. Christ, C. Messner, & L. Behard (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer. New York, NY: Oxford University Press.
Cupit-Link, M., Syrjala, K.L., & Hashmi, S.K. (2018). Damocles’ syndrome revisited: Update on the fear of cancer recurrence in the complex world of today’s treatments and survivorship. Hematology/Oncology and Stem Cell Therapy, 11, 129–134.
D’Urso, A., Mastroyannopoulou, K., & Kirby, A. (2017). Experiences of posttraumatic growth in siblings of children with cancer. Clinical Child Psychology and Psychiatry, 22, 301–317. https://doi.org/10.1177/1359104516660749
Dvorak, C.C., Gracia, C.R., Sanders, J.E., Cheng, E.Y., Baker, K.S., Pulsipher, M.A., & Petryk, A. (2011). NCI, NHLBI/PBMTC first international conference on late effects after pediatric hematopoietic cell transplantation: Endocrine challenges-thyroid dysfunction, growth impairment, bone health, and reproductive risks. Biology of Blood and Marrow Transplantation, 17, 1725–1738. https://doi.org/10.1016/j.bbmt.2011.10.006
Forsberg, M.H., Das, A., Saha, K., & Capitini, C.M. (2018). The potential of CAR T therapy for relapsed or refractory pediatric and young adult B-cell ALL. Therapeutics and Clinical Risk Management, 14, 1573–1584. https://doi.org/10.2147/tcrm.S146309
Foster, J.B., & Maude, S.L. (2018). New developments in immunotherapy for pediatric leukemia. Current Opinion in Pediatrics, 30, 25–29. https://doi.org/10.1097/mop.0000000000000572
Franco, V.I., & Lipshultz, S.E. (2015). Cardiac complications in childhood cancer survivors treated with anthracyclines. Cardiology in the Young, 25(Suppl. 2), 107–116.
Friedman, D.L. (2015). The ovary. In C.L. Schwartz, W.L. Hobbie, L.S. Constine, & K.S. Ruccione (Eds.), Survivors of childhood and adolescent cancer (3rd ed., pp. 253–265). Cham, Switzerland: Springer International.
Friedman, D.L., Whitton, J., Leisenring, W., Mertens, A.C., Hammond, S., Stovall, M., . . . Neglia, J.P. (2010). Subsequent neoplasms in 5-year survivors of childhood cancer: The Childhood Cancer Survivor Study. Journal of the National Cancer Institute, 102, 1083–1095.
Friedman, D.N., Hilden, P., Moskowitz, C.S., Suzuki, M., Boulad, F., Kernan, N.A., . . . Sklar, C.A. (2017). Cardiovascular risk factors in survivors of childhood hematopoietic cell transplantation treated with total body irradiation: A longitudinal analysis. Biology of Blood and Marrow Transplantation, 23, 475–482. https://doi.org/10.1016/j.bbmt.2016.12.623
Ginsberg, J.P. (2015). The testes. In C.L. Schwartz, W.L. Hobbie, L.S. Constine, & K.S. Ruccione (Eds.), Survivors of childhood and adolescent cancer (3rd ed., pp. 267–282). Cham, Switzerland: Springer International.
Giorgiani, G., Bozzola, M., Locatelli, F., Picco, P., Zecca, M., Cisternino, M., . . . Borrone, C. (1995). Role of busulfan and total body irradiation on growth of prepubertal children receiving bone marrow transplantation and results of treatment. Blood, 86, 825–831.
Grupp, S.A. (2014). Advances in T-cell therapy for ALL. Best Practice and Research. Clinical Haematology, 27, 222–228. https://doi.org/10.1016/j.beha.2014.10.014
Hobbie, W.L., Ogle, S.K., Reilly, M., Ginsberg, J.P., Rourke, M., Ratcliffe, S., & Deatrick, J.A. (2010). Identifying the educational needs of parents at the completion of their child’s cancer therapy. Journal of Pediatric Oncology Nursing, 27, 190–195.
Hucks, G., & Rheingold, S.R. (2019). The journey to CAR T cell therapy: the pediatric and young adult experience with relapsed or refractory B-ALL. Blood Cancer Journal, 10, 1–9.
Kadan-Lottick, N., & Kunin-Baston, A. (2015). Central nervous system effects In L. Schwartz, W. Hobbie, & L. Constine (Eds.), Survivors of childhood and adolescent cancer: A multi-disciplinary approach (3rd ed., pp. 43–63). Cham, Switzerland: Springer International.
Kazak, A.E., Barakat, L.P., Meeske, K., Christakis, D., Meadows, A.T., Casey, R., . . . Stuber, M.L. (1997). Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia. Journal of Consulting and Clinical Psychology, 65, 120–129.
Kenney, L.B., Laufer, M.R., Grant, F.D., Grier, H., & Diller, L. (2001). High risk of infertility and long term gonadal damage in males treated with high dose cyclophosphamide for sarcoma during childhood. Cancer, 91, 613–621.
Kreuser, E.D., Xiros, N., Hetzel, W.D., & Heimpel, H. (1987). Reproductive and endocrine gonadal capacity in patients treated with COPP chemotherapy for Hodgkin’s disease. Journal of Cancer Research and Clinical Oncology, 113, 260–266.
Krull, K.R., Brinkman, T.M., Chenghong, L., Armstrong, G.T., Ness, K.K., Srivastava, D.K., . . . Hudson, M.M. (2013). Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia. Journal of Clinical Oncology 31(35), 4407–4415.
Lamprecht, M., & Dansereau, C. (2019). CAR T-cell therapy: Update on the state of the science. Clinical Journal of Oncology Nursing, 23(2, Suppl.), 6–12.
Lawitschka, A., & Peters, C. (2018). Long-term effects of myeloablative allogeneic hematopoietic stem cell transplantation in pediatric patients with acute lymphoblastic leukemia. Current Oncology Reports, 20(9), 74. https://doi.org/10.1007/s11912-018-0719-5
Levine, J.M., Whitton, J.A., Ginsberg, J.P., Green, D.M., Leisenring, W.M., Stovall, M., . . . Sklar, C.A. (2018). Nonsurgical premature menopause and reproductive implications in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer, 124, 1044–1052.
Loughery, J., & Woodgate, R.L. (2015). Supportive care needs of rural individuals living with cancer: A literature review. Canadian Oncology Nursing Journal, 25, 157–178.
Maude, S.L., Teachey, D.T., Porter, D.L., & Grupp, S.A. (2015). CD19-targeted chimeric antigen receptor T-cell therapy for acute lymphoblastic leukemia. Blood, 125, 4017–4023.
Maus, M.V., Grupp, S.A., Porter, D.L., & June, C.H. (2014). Antibody-modified T cells: CARs take the front seat for hematologic malignancies. Blood, 123, 2625–2635.
Mazza, J.M., & Lin, S.Y. (2016). Primary immunodeficiency and recalcitrant chronic sinusitis: A systematic review. International Forum of Allergy and Rhinology, 6, 1029–1033.
Meadows, A.T., Gordon, J., Massari, D.J., Littman, P., Fergusson, J., & Moss, K. (1981). Declines in IQ scores and cognitive dysfunctions in children with acute lymphocytic leukaemia treated with cranial irradiation. Lancet, 2, 1015–1018.
Miedema, B., Easley, J., Fortin, P., Hamilton, R., & Mathews, M. (2008). The economic impact on families when a child is diagnosed with cancer. Current Oncology, 15(4), 8–13.
Mulhern, R.D., & Butler, R.W. (2004). Neurocognitive sequelae of childhood cancer and their treatment. Pediatric Rehabilitation, 7(1), 1–14.
National Cancer Institute. (2019). NCI dictionary of terms: Survivorship. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/survi…
Ogilvy-Stuart, A.L., Clark, D.L., Wallace, W.H., Gibson, B.E., Stevens, R.F., Shalet, S.M., & Donaldson, M.D. (1992). Endocrine deficit after fractionated total body irradiation. Archives of Disease in Childhood, 67, 1107–1110.
Orange, J.S., Grossman, W.J., Navickis, R.J., & Wilkes, M.M. (2010). Impact of trough IgG on pneumonia incidence in primary immunodeficiency: A meta-analysis of clinical studies. Clinical Immunology, 137, 21–30. https://doi.org/10.1016/j.clim.2010.06.012
Pelletier, W., & Bona, K. (2015). Assessment of financial burden as a standard of care in pediatric oncology. Pediatric Blood and Cancer, 62(Suppl. 5), S619–S631.
Rodriguez, E.M., Dunn, M.J., Zuckerman, T., Vannatta, K., Gerhardt, C.A., & Compas, B.E. (2012). Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology, 37, 185–197. https://doi.org/10.1093/jpepsy/jsr054
Rosenberg, A.R., Dussel, V., Kang, T., Geyer, J.R., Gerhardt, C.A., Feudtner, C., & Wolfe, J. (2013). Psychological distress in parents of children with advanced cancer. JAMA Pediatrics, 167, 537–543. https://doi.org/10.1001/jamapediatrics.2013.628
Shimazaki, S., Kazukawa, I., Ishida, M., & Minagawa, M. (2018). Thyroid nodules and long-term follow-up among childhood cancer survivors who underwent hematopoietic stem cell transplantation. Clinical Pediatric Endocrinology, 27, 75–79.
Smith, L., & Venella, K. (2017). Cytokine release syndrome: Inpatient care for side effects of CAR T-cell therapy. Clinical Journal of Oncology Nursing, 21(Suppl., 2), 29–34.
Stuber, M.L., Kazak, A.E., Meeske, K., Barakat, L., Guthrie, D., Garnier, H., . . . Meadows, A. (1997). Predictors of posttraumatic stress in childhood cancer survivors. Pediatrics, 100, 958–964.
Stuber, M.L., Meeske, K.A., Krull, K.R., Leisenring, W., Stratton, K., Kazak, A.E., . . . Zeltzer, L.K. (2010). Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics, 125, e1124–e1134. https://doi.org/10.1542/peds.2009-2308
Sulkers, E., Tissing, W.J., Brinksma, A., Roodbol, P.F., Kamps, W.A., Stewart, R.E., . . . Fleer, J. (2015). Providing care to a child with cancer: A longitudinal study on the course, predictors, and impact of caregiving stress. Psycho-Oncology, 24, 318–324.
van der Pal, H.J., van Dalen, E.C., van Delden, E., van Dijk, I.W., Kok, W.E., Geskus, R.B., . . . Kremer, L.C. (2012). High risk of symptomatic cardiac events in childhood cancer survivors. Journal of Clinical Oncology, 30, 1429–1437. https://doi.org/10.1200/JCO.2010.33.4730
Van Schoors, M., Caes, L., Alderfer, M.A., Goubert, L., & Verhofstadt, L. (2017). Couple functioning after pediatric cancer diagnosis: A systematic review. Psycho-Oncology, 26, 608–616.
Warner, E.L., Kirchhoff, A.C., Nam, G.E., & Fluchel, M. (2015). Financial burden of pediatric cancer for patients and their families. Journal of Oncology Practice, 11, 12–18.
Wei, C., & Crowne, E.C. (2018). The hypothalamic-pituitary-adrenal axis in childhood cancer survivors. Endocrine-Related Cancer, 25, R479–R496. https://doi.org/10.1530/ERC-18-0217
Wijnberg-Williams, B.J., Van de Wiel, H.B., Kamps, W., & Hoekstra-Weebers, J.E. (2015). Effects of communication styles on marital satisfaction and distress of parents of pediatric cancer patients: A prospective longitudinal study. Psycho-Oncology, 24, 106–112.
Wingard, J.R., Majhail, N.S., Brazauskas, R., Wang, Z., Sobocinski, K.A., Jacobsohn, D., . . . Socié, G. (2011). Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. Journal of Clinical Oncology, 29, 2230–2239.
Wohlschlaeger, A., Mostoufi-Moab, S., & Bunin, N. (2015). Hematopoietic stem cell transplantation. In C. Schwartz, W. Hobbie, L. Constine, & K. Ruccione (Eds.), Survivors of childhood and adolescent cancer (3rd ed., pp. 339–351). Cham, Switzerland: Springer International Publishing.
Yabroff, K.R., Lund, J., Kepka, D., & Mariotto, A. (2011). Economic burden of cancer in the United States. Cancer Epidemiology, Biomarkers, and Prevention, 20, 2006–2014.
Yang, H.C., Mu, P.F., Sheng, C.C., Chen, Y.W., & Hung, G.Y. (2016). A systematic review of the experiences of siblings of children with cancer. Cancer Nursing, 39(3), E12–E21.
Zhukovsky, D.S., Rozmus, C.L., Robert, R.S., Bruera, E., Wells, R.J., Chisholm, G.B., . . . Cohen, M.Z. (2015). Symptom profiles in children with advanced cancer. Cancer, 121, 4080–4087.




