Collaborative Care in Melanoma: The Essential Role of the Nurse
This article provides perspective from medical oncologists on the importance of this supplement from the Melanoma Nursing Initiative. The authors (a) delineate the challenges inherent in addressing adverse event (AE) management with newer melanoma therapies, particularly in the community setting; (b) illustrate how advanced practice providers with extensive clinical trial experience in melanoma are in a key position to set the agenda and educate colleagues on best practices in AE management; and (c) outline the rationale for the supplement and how it is uniquely tailored to enable community-based oncology nurses and allied health professionals caring for patients with melanoma to reduce the burden of AEs, support adherence, and improve patient outcomes.
AT A GLANCE
- Symptom/toxicity management is an issue of critical importance to patients with cancer.
- This initiative provided community-based oncology nurses with tools to reduce the burden of AEs, promote adherence, and support patients through the melanoma treatment journey.
- A collaborative approach to AE management should improve overall outcomes for patients with melanoma.
Jump to a section
This supplement to the Clinical Journal of Oncology Nursing features a series of consensus statements and tools developed by the members of the Melanoma Nursing Initiative (MNI) to empower oncology nurses in their efforts to improve outcomes associated with established and new molecularly targeted antitumor and immunologic therapies for melanoma. The treatment landscape for melanoma has changed dramatically, resulting in improved survival rates and disease outcomes for patients being treated in advanced and high-risk (adjuvant) settings (Andtbacka et al., 2015; Bendell et al., 2017; Eggermont et al., 2015, 2016; Larkin et al., 2014, 2015; Robert, Long, et al., 2015; Robert, Schachter, et al., 2015). Disease and survival outcomes are likely to improve as newer therapies become available, combination therapy approaches evolve, and the ability to tailor treatment and address challenges, such as brain metastases, continue to expand.
Although the promise of improved survival and disease outcomes drives the research agenda, healthcare providers must not lose sight of an outcome of critical importance to patients—symptom/toxicity management. As a group, oncologists do not focus extensively on this issue (Okuyama et al., 2011; Shin et al., 2011). Efforts are often focused on the general benefit-risk assessment and the primary treatment goal of improved overall and disease-free survival. However, survival can be compromised if adverse events (AEs) are left untreated so that they progress sufficiently in severity (i.e., become life-threatening), cause nonadherence, or trigger treatment discontinuation (Boutros et al., 2016; Timmers et al., 2014; Villadolid & Amin, 2015). Therefore, prompt recognition and optimal management of AEs is an essential requirement for achievement of all treatment outcomes.
One of the challenges in addressing the AEs of newer melanoma therapies is related to experience and knowledge transfer. These melanoma therapies are associated with a range of AEs that differ from those associated with chemotherapy. Working with these therapies requires a complete shift in thinking for nurses accustomed to dealing with chemotherapy AEs. Nurses with expertise in melanoma have a wealth of experience with the newer therapies, expertise that they started developing over the course of clinical trials with these agents. As members of expert tertiary care teams, nurses have additional real-world, post-approval experience with these agents and can share that experience directly with other nursing and allied healthcare professionals in their networks and cooperative groups.
Unfortunately, outside the walls of the academic melanoma center, such expertise is frequently lacking. For example, in the melanoma clinical trials that the current authors have conducted in conjunction with community affiliate sites, numerous questions about how to manage AEs have been fielded despite the availability of a protocol. In addition, many MNI nursing colleagues can attest to the number of questions they receive from oncologists and nurses alike about how to recognize and manage the unique AEs associated with these targeted and immunologically based therapies for melanoma. The need for guidance is palpable in the community setting.
The MNI is uniquely designed to provide community-based oncology nurses and allied healthcare teams with the necessary tools to promote adherence; reduce the burden of AEs; and support patients, families, and caregivers through the melanoma treatment journey. The MNI members are a distinguished group of multidisciplinary healthcare providers with expertise in melanoma (see Figure 1). They have developed a set of care step pathways to guide fellow oncology nurses via strategies to educate patients, promote adherence, and provide nursing assessment and AE management. The steps they propose can make a big difference in the lives of patients. Such comprehensive nursing assessments and interventions have not been addressed in the myriad guideline publications on AE management for melanoma therapies. In addition, under the leadership of Valerie Guild, co-founder and president of the AIM at Melanoma Foundation, this initiative puts practical educational materials and resources in the hands of the other important oncology stakeholder—the patient with melanoma. The MNI website (www.themelanomanurse.org) features many of the tools and resources published in this supplement as well as practical, up-to-date, downloadable patient resources.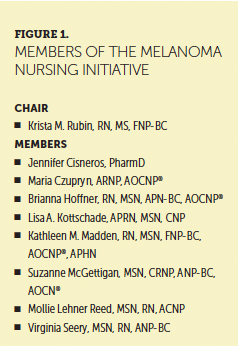
The MNI’s goal is for the resources provided to be shared among oncology care groups and collaborating allied healthcare providers to spark opportunities for propagating further regionally based, peer-to-peer education. The current authors anticipate sharing these resources with in-house nurse experts for use in educating oncology nursing peers within the community and hope that readers of this supplement will do the same to further the goal of improving patient outcomes.
About the Author(s)
John M. Kirkwood, MD, is the Usher Professor of Medicine, Dermatology, and Translational Science and director of the Melanoma and Skin Cancer Program in the School of Medicine at the University of Pittsburgh in Pennsylvania; and Antoni Ribas, MD, PhD, is a professor of medicine, surgery, and molecular and medical pharmacology and director of the Tumor Immunology Program at the University of California, Los Angeles Jonsson Comprehensive Cancer Center. The authors take full responsibility for this content. This supplement was funded by the AIM at Melanoma Foundation, with support via unrestricted grants from Amgen, Array Biopharma, Bristol-Myers Squibb, Incyte Corporation, Merck and Co., and Novartis Pharmaceuticals. Writing and editorial support was provided by Lisa A. Tushla, PhD, H(ASCP), at Terranova Medica. During the writing of this article, Kirkwood was supported by research funding from Prometheus and Merck and Co. and has received fees for participation in advisory or review activities from Amgen, Bristol-Myers Squibb, Checkmate Pharmaceuticals, Green Peptide, Novartis Pharmaceuticals, Roche, and Solaran RX. During the writing of this article, Ribas was supported by grants (R35 CA197633; P01 CA168585; 1U54 CA199090; R01 CA170689) from the National Cancer Institute/National Institutes of Health, the Parker Institute for Cancer Immunotherapy, the Ressler Family Foundation, the Dr. Robert Vigen Memorial Fund, the Grimaldi Family Fund, the Samuels Family Fund, the Garcia-Corsini Family Fund, and a Stand Up To Cancer–Cancer Research Institute (SU2C-CRI) Cancer Immunology Dream Team Translational Research Grant (SU2C- AACR-DT1012). Ribas has previously received fees for participation on advisory boards from Amgen, Celldex, Merck and Co., and Novartis Pharmaceuticals. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Kirkwood can be reached at kirkwoodjm@upmc.edu, with copy to CJONEditor@ons.org. (Submitted April 2017. Accepted May 23, 2017.)
References
Andtbacka, R.H., Kaufman, H.L., Collichio, F., Amatruda, T., Senzer, N., Chesney, J., . . . Coffin, R.S. (2015). Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. Journal of Clinical Oncology, 33, 2780–2788. doi:10.1200/jco.2014.58.3377
Bendell, J.C., Javle, M., Bekaii-Saab, T.S., Finn, R.S., Wainberg, Z.A., Laheru, D.A., . . . Patnaik, A. (2017). A phase 1 dose-escalation and expansion study of binimetinib (MEK162), a potent and selective oral MEK1/2 inhibitor. British Journal of Cancer, 116, 575–583. doi:10.1038/bjc.2017.10
Boutros, C., Tarhini, A., Routier, E., Lambotte, O., Ladurie, F.L., Carbonnel, F., . . . Robert, C. (2016). Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nature Reviews Clinical Oncology, 13, 473–486. doi:10.1038/nrclinonc.2016.58
Eggermont, A.M., Chiarion-Sileni, V., Grob, J.J., Dummer, R., Wolchok, J.D., Schmidt, H., . . . Testori, A. (2015). Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): A randomised, double-blind, phase 3 trial. Lancet Oncology, 16, 522–530. doi:10.1016/S1470-2045(15)70122-1
Eggermont, A.M., Chiarion-Sileni, V., Grob, J.J., Dummer, R., Wolchok, J.D., Schmidt, H., . . . Testori, A. (2016). Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. New England Journal of Medicine, 375, 1845–1855. doi:10.1056/NEJMoa1611299
Larkin, J., Ascierto, P.A., Dreno, B., Atkinson, V., Liszkay, G., Maio, M., . . . Ribas, A. (2014). Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. New England Journal of Medicine, 371, 1867–1876. doi:10.1056/NEJMoa1408868
Larkin, J., Chiarion-Sileni, V., Gonzalez, R., Grob, J.J., Cowey, C.L., Lao, C.D., . . . Wolchok, J.D. (2015). Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. New England Journal of Medicine, 373, 23–34. doi:10.1056/NEJMoa1504030
Okuyama, T., Akechi, T., Yamashita, H., Toyama, T., Nakaguchi, T., Uchida, M., & Furukawa, T.A. (2011). Oncologists’ recognition of supportive care needs and symptoms of their patients in a breast cancer outpatient consultation. Japanese Journal of Clinical Oncology, 41, 1251–1258. doi:10.1093/jjco/hyr146
Robert, C., Long, G.V., Brady, B., Dutriaux, C., Maio, M., Mortier, L., . . . Ascierto, P.A. (2015). Nivolumab in previously untreated melanoma without BRAF mutation. New England Journal of Medicine, 372, 320–330. doi:10.1056/NEJMoa1412082
Robert, C., Schachter, J., Long, G.V., Arance, A., Grob, J.J., Mortier, L., . . . Ribas, A. (2015). Pembrolizumab versus ipilimumab in advanced melanoma. New England Journal of Medicine, 372, 2521–2532. doi:10.1056/NEJMoa1503093
Shin, D.W., Kim, S.Y., Cho, J., Sanson-Fisher, R.W., Guallar, E., Chai, G.Y., . . . Park, J.H. (2011). Discordance in perceived needs between patients and physicians in oncology practice: A nationwide survey in Korea. Journal of Clinical Oncology, 29, 4424–4429. doi:10.1200/JCO.2011.35.9281
Timmers, L., Boons, C.C., Kropff, F., van de Ven, P.M., Swart, E.L., Smit, E.F., . . . Hugtenburg, J.G. (2014). Adherence and patients’ experiences with the use of oral anticancer agents. Acta Oncologica, 53, 259–267. doi:10.3109/0284186X.2013.844353
Villadolid, J., & Amin, A. (2015). Immune checkpoint inhibitors in clinical practice: Update on management of immune-related toxicities. Translational Lung Cancer Research, 4, 560–575. doi:10.3978/j.issn.2218-6751.2015.06.06




